Session Information
Date: Sunday, November 8, 2020
Title: Sjögren’s Syndrome Poster
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Mast cells have been implicated in many immune-inflammatory disorders. They mediate a variety of inflammatory and fibrotic conditions, but their role in sialadenitis in patients with primary Sjögren’s syndrome (pSS) is unclear. We examined whether mast cells play a critical role in the pathogenesis of pSS.
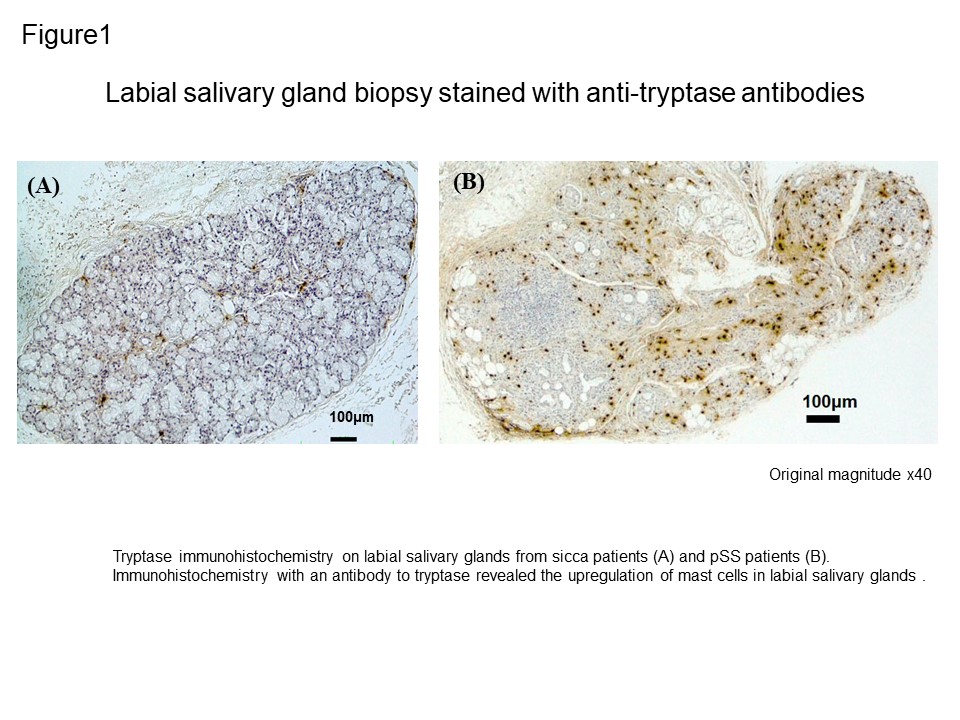
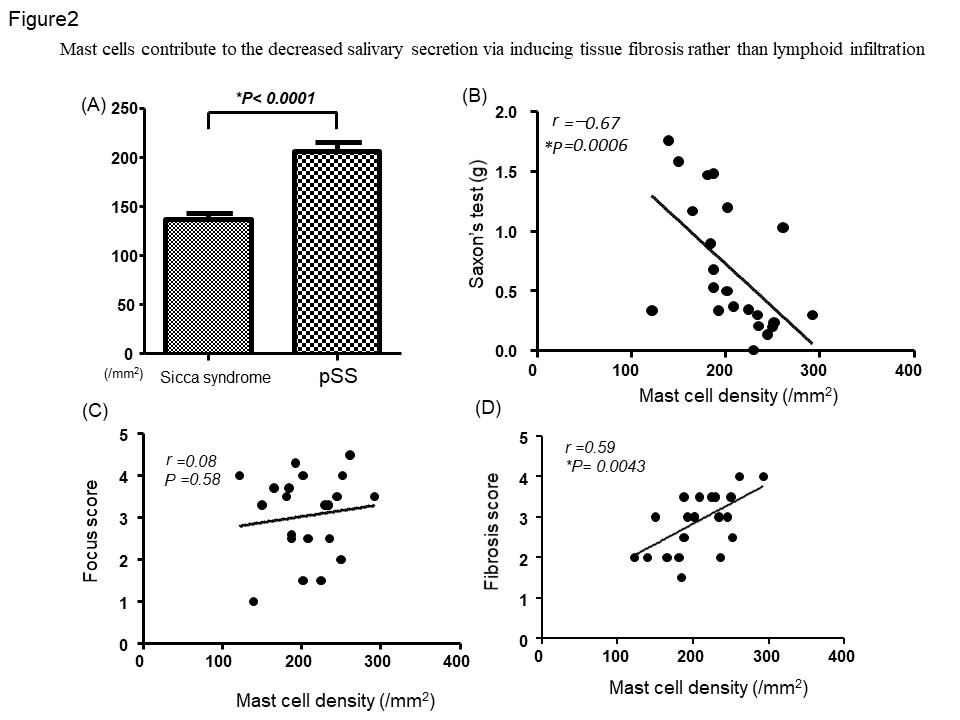
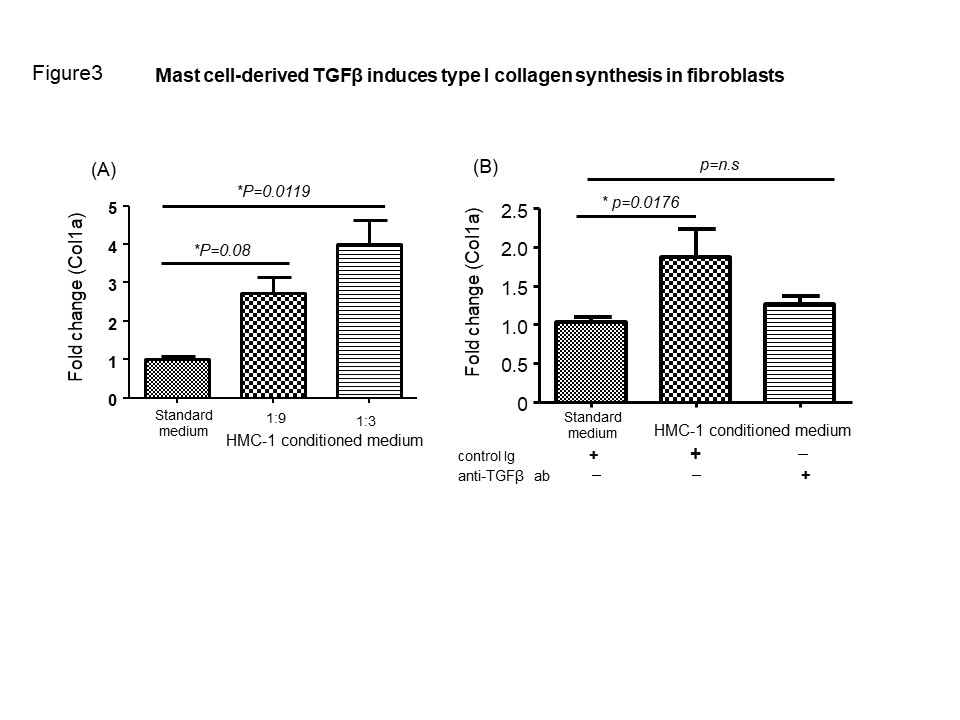
Methods: Labial salivary gland samples were collected from 22 individuals with pSS and 10 with sicca syndrome (controls). Saliva production was evaluated by Saxon’s test. Mast cell density in minor salivary glands was calculated at 400 magnification. The degree of fibrosis in minor labial salivary gland was graded on a quantitative scale as previously reported (Clin Exp Rheumatol.1998;16:63-65). We used immunohistochemistry to identify and quantify tryptase or TGFβ-positive mast cells and vimentin-positive fibroblasts. Fibrous tissue was identified by using EVG stain. Conditioned medium for fibroblast culture was obtained from human mast cell line-1 (HMC-1 )cells stimulated with recombinant human IL-33 and SCF for 24 hours. Fibroblasts were treated with HMC-1 conditioned medium for 24 hours and type I collagen synthesis in fibroblast was evaluated by RT-qPCR. Neutralization antibodies for human TGFβ was utilized during fibroblast culture with HMC-1 conditioned medium or standard culture medium.
Results: We found that the number of mast cells in labial salivary glands of patients with pSS was significantly increased compared to that in control subjects (Figure 1 and Figure 2A). There was a significant negative correlation between the Saxon’s test results and the number of mast cells, suggesting the involvement of mast cells in the decreased salivary secretion (Figure 2B). There was no correlation between the intensity of lymphoid infiltration assessed by focus score and the mast cell density (Figure 2C). In contrast, a significant correlation between the number of mast cells and the degree of fibrosis was observed (Figure 2D). Consistent with these findings, mast cells were proximal to EVG-stained fibrous tissue and vimentin-positive fibroblasts. We hypothesized that mast cells were involved in the development of tissue fibrosis via modulation of fibroblast immune function. Significant up-regulation of Col1a mRNA was observed in fibroblast with HMC-1 conditioned medium as inverse proportion to the degree of dilution compared to that of fibroblast with standard culture medium (Figure 3A). Furthermore, neutralization for TGFβ abolished upregulation of Col1a mRNA in fibroblast in HMC-1 conditioned medium, thus suggesting that HMC-1-derived TGFβ contributes to upregulation of type I collagen synthesis (Figure 3B). Immunohistochemistry revealed that tryptase-positive mast cells exhibited positive signal of TGFβ in serial section.
Conclusion: These results suggest a novel role for mast cells in the development of sialadenitis in patients with pSS by induction of tissue fibrosis via fibroblast collagen synthesis by TGFβ production.
To cite this abstract in AMA style:
Kaieda S, Fujimoto K, Ida H. Mast Cells Contribute to the Development of Sialadenitis Associated with Sjögren’s Syndrome via Inducing Tissue Fibrosis by TGFβ Production [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/mast-cells-contribute-to-the-development-of-sialadenitis-associated-with-sjogrens-syndrome-via-inducing-tissue-fibrosis-by-tgf%ce%b2-production/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/mast-cells-contribute-to-the-development-of-sialadenitis-associated-with-sjogrens-syndrome-via-inducing-tissue-fibrosis-by-tgf%ce%b2-production/