Session Information
Date: Sunday, November 8, 2020
Title: Pediatric Rheumatology – Clinical Poster II: Systemic JIA, Autoinflammatory, & Scleroderma
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: STING-Associated Vasculopathy with Onset in Infancy (SAVI) is an autoinflammatory interferonopathy caused by gain-of-function mutations in STING1, characterized by peripheral vasculopathy and interstitial lung disease. Our aim is to describe the clinical and immunological manifestations of SAVI.
Methods: Clinical information on 33 patients with SAVI, based on NIH evaluation (n=15) or on records and samples provided by collaborators (n=18), were retrospectively reviewed. Patients were enrolled in an IRB-approved natural history protocol. The IFN score was calculated as previously described [1]. Features of lung inflammation and damage on Computed Tomography (CT) were scored by a single radiologist (LF). Severe lung disease was defined as presence of at least one characteristic: lung fibrosis, respiratory insufficiency, pulmonary hypertension, or digital clubbing associated with interstitial lung disease on chest CT.
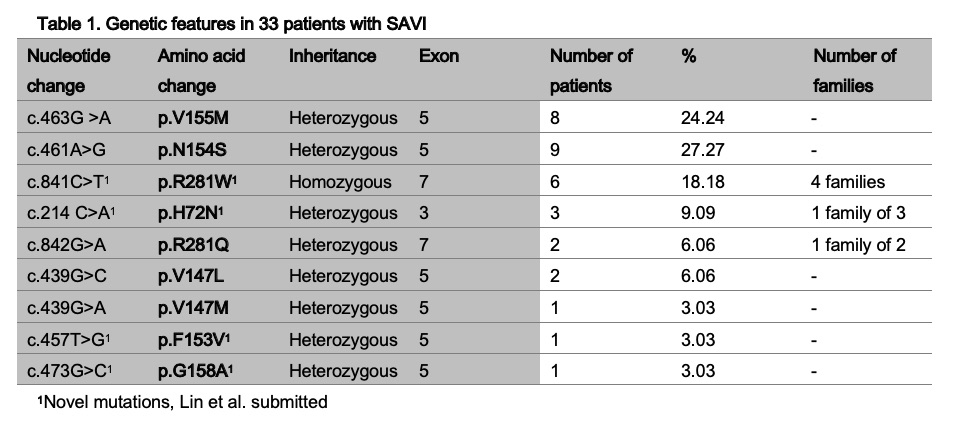
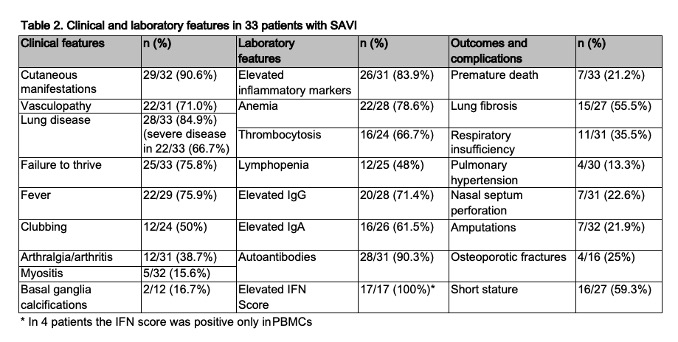
Results: 13/33 (39.4%) patients were female. SAVI was sporadic in 73% and familial in 27%. Heterozygous mutations were disease-causing in 81.8%, however, a p.R281W mutation, present in 6 patients from 4 families, required homozygosity (additive gain-of-function). The p.N154S and p.V155M mutations were most common (27.3% and 24.2% respectively, see Table 1). Disease symptoms presented in the first year of life (75%), with rash (18/31), respiratory symptoms (13/31) and fever (11/31). Table 2 lists clinical and laboratory features in SAVI. The p.N154S mutation is associated with vasculopathy (p=0.03); patients with the p.V155M mutation tend to have more severe lung disease (p=0.2). Median age at last evaluation was 12 years (range 0.4-54.1). 7 patients died at a mean age of 7 years (range 0.4-15); due to respiratory failure n=4, multiorgan failure n=1, sepsis n=1, unknown n=1. In 4/17 the IFN score was negative in whole blood, but positive in PBMCs. Patients failed a mean of 2.1 DMARDs or biologics, 76.6% received steroids. 25 patients were treated with a JAK-inhibitor (baricitinib n=14, tofacitinib n=7, ruxolitinib n=7), for an average of 2.1 years (range 0-5.7). Skin ulcers improved in 10/10, but recurred. Over an average of 2.6 years (range 1.1-3.9), on chest CT, features of inflammation improved in 6/7, with stable/improved damage in 6/7.
Conclusion: SAVI is a severe early-onset interferonopathy, that can lead to amputations, respiratory insufficiency and premature death. SAVI is sporadic in 73%. Most pathogenic STING1 mutations are heterozygous, except for p.R281W, which is disease-causing in homozygosity. With the absence of peripheral disease in 9.4%, SAVI should be suspected in any patient with interstitial lung disease even in the absence of vasculopathy. The p.N154S mutation is associated with vasculopathy, and the p.V155M with more severe lung disease. Rarely, the IFN score can be negative in whole blood and positive in PBMCs. Treatment with JAK inhibitors halted progression of lung damage over an average of 2.3 years, but only partially controlled peripheral vasculopathy and did not normalize the IFN score.
Funding for this study was provided by the Division of Intramural Research, NIAID, NIH
- Kim et al. J Interferon Cytokine Res 2018;38:171–85
To cite this abstract in AMA style:
Torreggiani S, Alehashemi S, Mitchell J, Souto Adeva G, Lin B, Wade J, Montealegre Sanchez G, Alrasheed A, Balci S, Berard R, Arturo B, Brunner J, Buehring B, Buthaina A, Cancrini C, Carter J, Corbeto Lopez M, De Benedetti F, Do H, Dueckers G, Folio L, Insalaco A, Kisla Ekinci R, Miller M, Montes Cano M, Morin M, Ozen S, Pacillo L, Ramsey S, Reinhardt A, Rumsey D, Santiago L, Schulert G, Wright B, de Jesus A, Goldbach-Mansky R. Clinical Features and Outcomes in STING-Associated Vasculopathy with Onset in Infancy (SAVI) [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/clinical-features-and-outcomes-in-sting-associated-vasculopathy-with-onset-in-infancy-savi/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-features-and-outcomes-in-sting-associated-vasculopathy-with-onset-in-infancy-savi/