Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Lumbar spinal stenosis (LSS) is a disabling condition, mostly prevalent in the aging population and associated with significant healthcare cost. Clinical presentation involving neurogenic claudication and low back pain results from congenital or degenerative narrowing of the spinal canal. Greater narrowing of the lumbar spinal canal has been described in African which contrasts with a lower incidence of the condition in this population. In clinical trials and meta-analysis of LSS treatment, the majority of the study populations are of Caucasian origin, accounting for 70% to 95% of the patients1,2,3. No difference between surgery, physiotherapy or epidural corticosteroid injection in LSS has been reported in those studies. To our knowledge, none has been performed in Afro-descendant populations (AD). We aim to assess efficacy of 3 different treatment approaches for lumbar spine stenosis in Martinique, a French Caribbean island with a high level of care in the region and an aging population mostly composed of AD.
Methods: Prospective cohort of 138 Afro-Caribbean patients with LSS, evaluated at 3 months from a first course of epidural corticosteroid injections in combination with standardized physiotherapy then assigned to 3 arms of treatment according to clinical evolution and wishes: rehabilitation (R: physiotherapy and oral medication), second course of epidural corticosteroid injections (ECI) or decompression surgery (DS). The primary endpoint was change in Oswestry Disability index (ODI) at 3 months (M3), M12, M18, M24. Secondary endpoints were change in leg pain and back pain measured by Visual Analog Scale (respectively L-VAS and B-VAS).
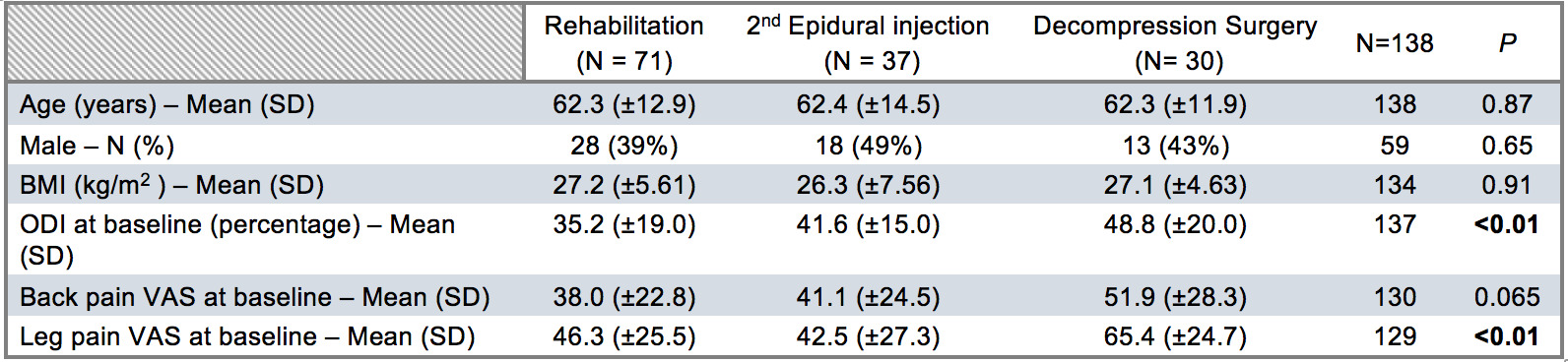
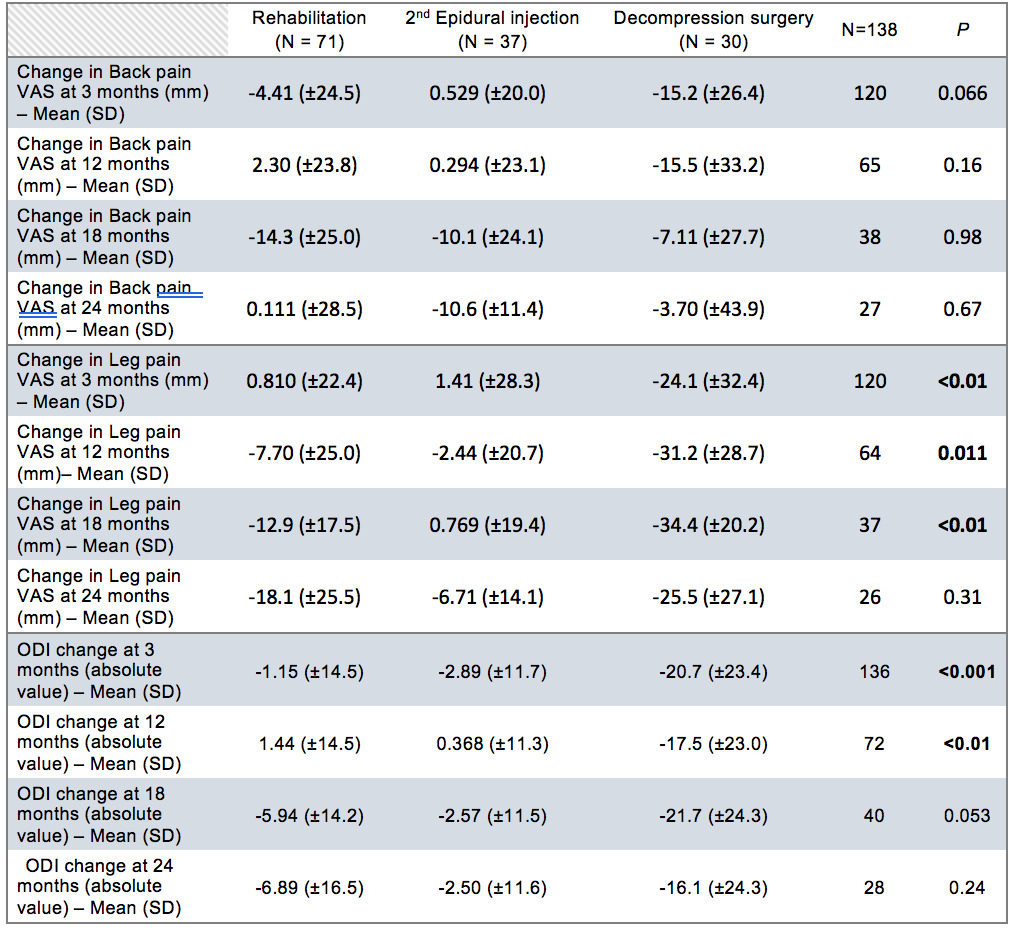
Results: Seventy-one patients were assigned to the R arm, 37 to the second ECI arm, 30 patients to the DS arm. All arms were comparable in age (62.3 +/- 13.1 years), sex (male/female ratio 0.75) and BMI with an average of 27.0 +/- 5.97 kg/m2. ODI and L-VAS were significantly higher in the DS arm at baseline (p< 0.01). No difference in B-VAS was observed at baseline (Table1). A significantly higher decrease in ODI was observed in the DS arm at M3 and M12 (respectively P< 0.001 and P< 0.01). Results were not replicated at M18 and M24. A significantly higher decrease in L-VAS was observed in the DS arm at M3, M12, M18 (respectively P< 0.01, P=0.011, P< 0.01), not replicated at M24. No difference was observed between the 3 arms for B-VAS at no time (Table 2).
Conclusion: This is the first comparative treatment study in LSS performed in an AD population. We report a significant superiority of DS in evolution of ODI, a composite functional score, and L-VAS at M3 and M12. These results are very similar to those of major studies comparing surgical to non-surgical therapies for LSS in Caucasian cohorts2,3. If long terms (M24) favorable outcomes of L-VAS and ODI is not replicated in our study contrary to others, there is clearly a tendency in favor of surgery. Absence of statistical significance could be explained by important loss to follow up.
References
- Zaina F et al. , Cochrane Database Syst Rev. 2016(1):CD010264.
- Delitto A et al. , Ann Intern Med. 2015;162(7):465-73.
- Malmivaara A et al. , Spine (Phila Pa 1976). 2007;32(1):1-8.
To cite this abstract in AMA style:
Louis-sidney F, Arfi S, Drame M, Deligny C, Cabre P, de Bandt M. Lumbar Spine Stenosis Treatment : Is Surgery Better Than Medical Treatment in Afro-Descendant Populations ? [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/lumbar-spine-stenosis-treatment-is-surgery-better-than-medical-treatment-in-afro-descendant-populations/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/lumbar-spine-stenosis-treatment-is-surgery-better-than-medical-treatment-in-afro-descendant-populations/