Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Prior studies of calcium pyrophosphate crystal deposition disease (CPPD) epidemiology either focused on the entire spectrum of CPPD or identified patients with its acute manifestation, pseudogout, using single non-validated diagnosis codes. We investigated previously identified risk factors for CPPD or pseudogout—including bisphosphonates, diuretics, osteoarthritis, and hyperparathyroidism—among well-defined pseudogout patients.
Methods: We performed a case-control study by applying a validated algorithm to identify pseudogout cases using electronic medical record (EMR) data (PPV 81%) at an academic medical center. Case index date was the earlier of 1st positive synovial fluid calcium pyrophosphate crystal analysis or 1st natural language processing concept “pseudogout” in narrative notes. Cases were matched to up to 4 general EMR controls not classified as pseudogout by the algorithm. Matching occurred on year of 1st EMR encounter and index date (encounter ±30d of case index date). We required age ≥50 at index date and ≥2 encounters in the 365 days before index date for cases and controls. We pre-specified covariates of interest: (1) comorbidities previously associated with CPPD in the literature, identified by ≥1 billing code from 1st EMR encounter through index date and (2) prescriptions for medications previously associated with CPPD in the literature, recorded in the 90 days prior to and including index date. A multimorbidity score was calculated for each patient using a validated method based on billing codes for 40 conditions. A multivariable logistic regression model estimated the odds ratio (OR) and 95% CI for each pre-specified covariate adjusted for age, total number of encounters from 1st EMR encounter through index date, multimorbidity score, and all pre-specified covariates.
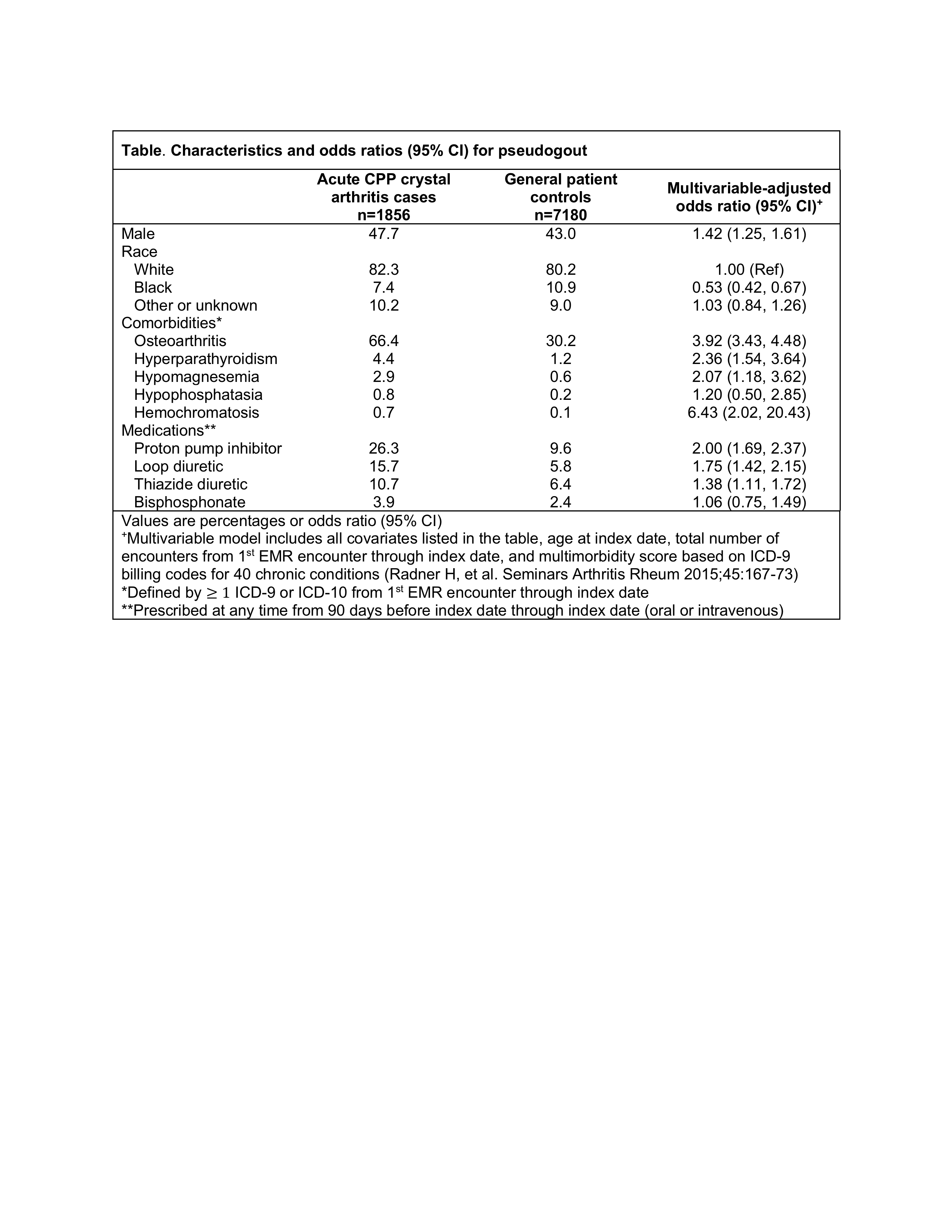
Results: We identified 1856 cases matched to 7180 controls. Mean age was 73 years, 56.0% were female, 80.6% white, 10.2% black, and 9.2% other/unknown race. Among pseudogout patients, 12.8% were age 50-59, 25.9% age 60-69, 31.7% age 70-79, and 29.6% age ≥80. Each of the pre-specified covariates were more common in pseudogout cases than controls (Table). Risk for pseudogout was significantly higher for patients with osteoarthritis (OR 3.92), male sex (OR 1.42), proton pump inhibitors (OR 2.00), loop diuretics (OR 1.75), thiazides (OR 1.38), and rare metabolic disorders including hyperparathyroidism, hypomagnesemia, and hemochromatosis. Bisphosphonates were not significantly associated with pseudogout. Black race was associated with significantly lower risk for pseudogout compared to white race (OR 0.53).
Conclusion: Using a validated algorithm to identify >1800 pseudogout cases, we identified important metabolic correlates of this acute manifestation of CPPD. This is the first study to report higher risk for pseudogout among men and lower risk among black compared to white patients. We confirmed several previously published risk factors, but in contrast to prior studies we did not identify an association between bisphosphonates and pseudogout.
To cite this abstract in AMA style:
Tedeschi S, Yoshida K, Huang W, Solomon D. Risk Factors for Pseudogout: An Electronic Medical Record Case-Control Study [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/risk-factors-for-pseudogout-an-electronic-medical-record-case-control-study/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-factors-for-pseudogout-an-electronic-medical-record-case-control-study/