Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Recent experimental data suggest in utero exposure to maternal antibodies and cytokines as important risk factors for autism spectrum disorders (ASD). Interestingly, women with SLE display autoantibodies (e.g. anti-N-methyl-D-aspartate receptor and antiphospholipid antibodies) and cytokines (e.g. interleukin-6), which, in animal models, alter fetal brain development and induce behavioural anomalies in offspring. To date, no one has specifically assessed the risk of ASD in children of SLE mothers. Using the “Offspring of Systemic Lupus Erythematosus mothers Registry (OSLER)”, we aimed to determine if children born to SLE mothers have an increased risk of ASD compared to children born to mothers without SLE.
Methods: OSLER is a large population-based cohort, which includes all women who had ³1 hospitalization for delivery after SLE diagnosis, identified through Quebec’s universal healthcare databases (1989-2009). OSLER also includes a randomly selected control group of women, matched at least 4:1 for age and year of delivery, who did not have a diagnosis of SLE prior to or at the time of delivery. We identified children born live to SLE mothers and their matched controls, and ascertained ASD based on ³1 hospitalization or physician visit with a relevant diagnostic code, through to end of database follow-up.
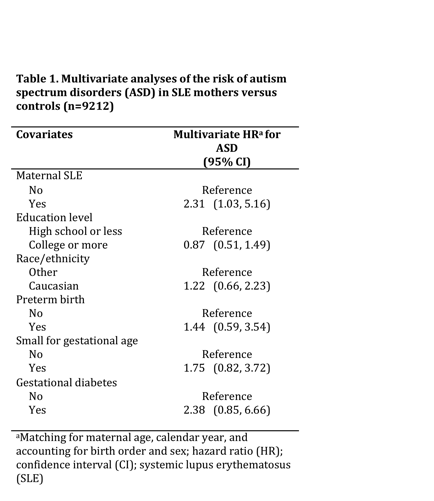
We performed multivariate analyses to adjust for maternal demographics, sex and birth order of child, and obstetrical complications. In a subsample analysis of children with maternal public drug coverage throughout pregnancy, we further assessed relevant in utero medication exposures.
Results: 509 women with SLE had 719 children, while 5824 matched controls had 8493 children. Mean maternal age and follow-up were respectively 30.3 [standard deviation (SD) 5.0] and 9.1 (SD 5.8) years. Children born to women with SLE had more records of ASD diagnoses compared to controls [1.4% (95% CI 0.8, 2.5) vs 0.6% ( 95%CI 0.5, 0.8)]. Mean age at ASD diagnosis was slightly younger in offspring of SLE mothers (3.8 years, 95%CI 1.8, 5.8) as opposed to controls (5.7 years, 95%CI 4.9, 6.5).
In multivariate analyses (Table 1), children born to women with SLE had substantially increased risk of ASD versus controls (HR 2.31, 95%CI 1.03, 5.16). In the subsample of children with maternal drug coverage (n=1925), in utero medication exposures were rare in the 18 ASD cases: none were exposed to antimalarials, antidepressants, or immunosuppressants, while only one case born to a SLE mother and another born to a control mother were respectively exposed to corticosteroids and anticonvulsants.
Conclusion: Compared to children from the general population, children born to women with SLE have a substantially increased risk of ASD. Our findings are supported by previous experimental data and should prompt further research on the potential role of SLE-related autoantibodies, such as N-methyl-D-aspartate receptor antibodies, in ASD.
Disclosure:
E. Vinet,
None;
S. Scott,
None;
C. A. Pineau,
None;
L. Joseph,
None;
A. E. Clarke,
None;
E. Fombonne,
None;
R. W. Platt,
None;
S. Bernatsky,
None.
« Back to 2013 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/increased-risk-of-autism-spectrum-disorders-in-children-born-to-women-with-sle-preliminary-data-from-the-o-s-l-e-r-cohort/