Session Information
Date: Saturday, November 7, 2020
Title: Epidemiology & Public Health Poster II: OA, Osteoporosis, & Other Rheumatic Disease
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: The long-term safety of breast implants has been a debated topic; two recent studies have raised new concerns about their potential negative health effects (Watad A et al., Int J Epidemiol. 2018; Coroneos C et al., Annals of Surgery. 2018). While these reports suffer from methodological weaknesses, previous studies indicating no association between silicone breast implants and systemic disease may have been under-powered for rare outcomes. Since disease diagnostic criteria have been expanded in modern times, we felt these recent reports required a re-examination of whether autoimmune conditions occurred more frequently in women after silicone and saline breast implantation compared to those with no history of implants.
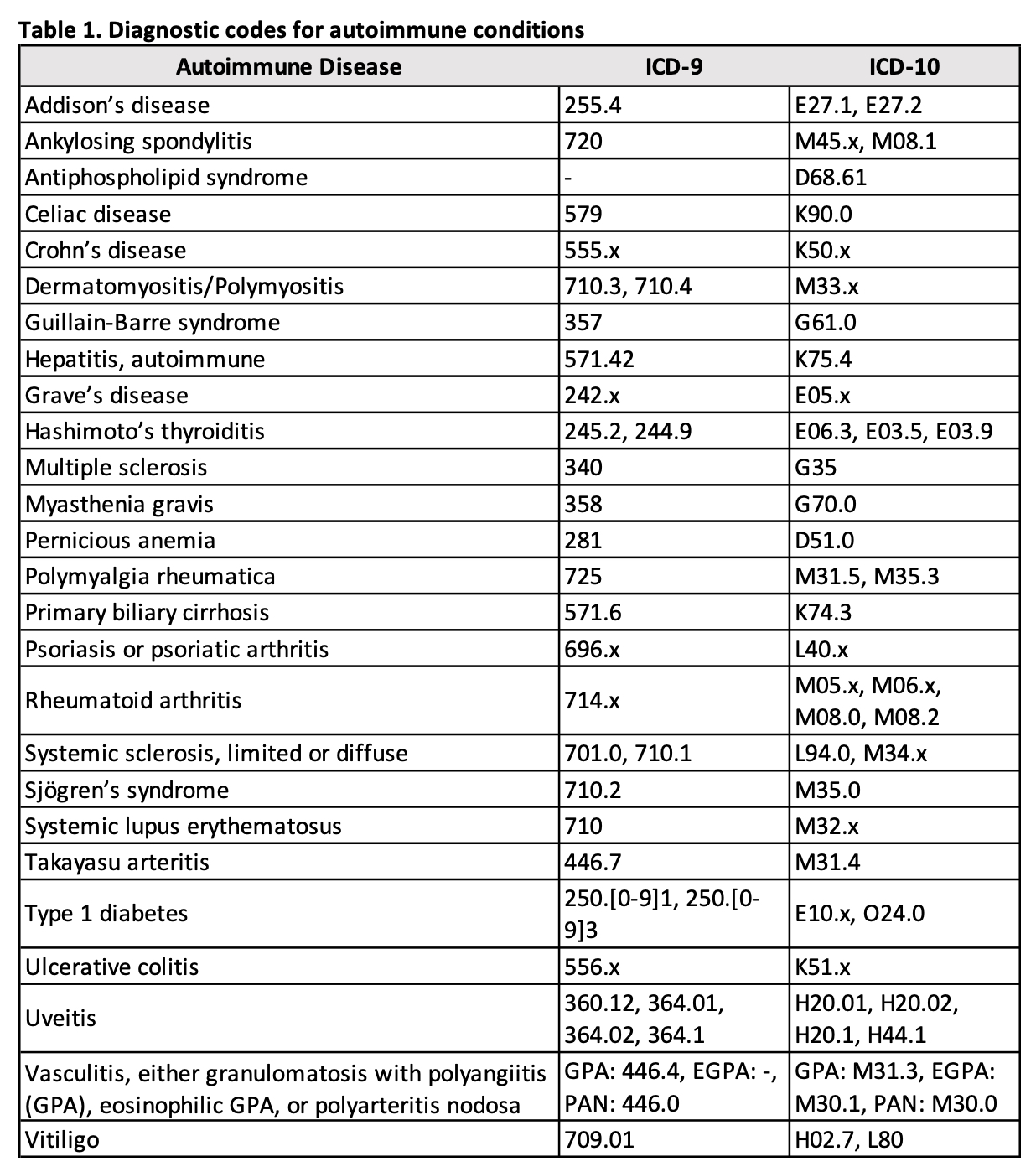
Methods: In this retrospective cohort study, all women who received a breast implant in a geographically defined region between January 1, 1998 and December 31, 2017 were identified. Implant cases were individually reviewed to confirm implant status and determine implant date, type, and reason. Each subject was matched to 3 women of the same age and region with no history of implants. Index date was defined as date of implantation or matched date. Both cohorts were screened for 26 autoimmune conditions using diagnostic codes (Table 1). Using a previously validated method, confirmed autoimmune conditions were defined by the presence of ≥1 inpatient encounter as the primary diagnosis, or ≥2 codes ≥30 days and ≤2 years apart (Ong MS et al., JAMA Neurol. 2014). Comparisons of autoimmune disease occurrence in women with and without implants were performed using Cox models adjusted for age and calendar year.
Results: We identified 835 women who received breast implants during the study period and 2505 comparators with no history of implants. Women with implants were 89.2% white with a mean age of 41.4 years at implantation. Roughly half the implants were for cosmetic reasons (n = 422; 50.5%), with 310 (37.1%) for breast cancer, and 103 (12.3%) for prophylaxis or reasons related to another condition. The median length of prior medical history for implant patients was 24.9 years (IQR: 11.3, 36.1). After implant placement, these women had a median follow-up of 9.3 years (IQR: 4.8, 14.2). Prior to receiving implants, 129 (15.4%) women had an autoimmune condition compared to 381 (15.2%) comparators (p = 0.87). Excluding women with prior autoimmune disease, 74 women with implants (cumulative incidence at 10 years: 11.0%; 95% CI: 8.5-14.1%) and 222 comparators (cumulative incidence at 10 years: 11.3%; 95% CI: 9.8-13.0%) developed an autoimmune condition during follow-up. We found no evidence of an increase in the risk of autoimmune disease for women with implants compared to those without (HR: 0.98; 95% CI: 0.75-1.27). When assessing the risk of autoimmune disease for implant reason subtypes, we did not observe any differences (Table 2).
Conclusion: This study observed no increase in the modern era for the risk of autoimmune diseases in women with breast implants compared to those without. Additional analyses are currently underway for saline vs. silicone subsets as well as analyses focusing on length of implant exposure.
To cite this abstract in AMA style:
Peterson M, O'Byrne T, Davis J, Kronzer V, Peterson L, Weisman M, Crowson C. Autoimmune Disease Outcomes of Women with Breast Implants: A Population-Based Study [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/autoimmune-disease-outcomes-of-women-with-breast-implants-a-population-based-study/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/autoimmune-disease-outcomes-of-women-with-breast-implants-a-population-based-study/