Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Diagnosis of the central nervous system vasculitis (CNS-V) is made on the basis of image findings or brain biopsy. Recently, two different subtypes of the disease have been postulated, the small (SVV) and large-medium vessel variant (LMVV). We hypothesized that the image profiles and diagnostic approaches would vary between the LMVV and the SVV in patients with CNS-V. The aim of this study was to clarify the clinical characteristics, brain MRI findings, and diagnostic accuracy for high-resolution vessel wall image (HR-VWI) and brain biopsy according to affected vessel size in CNS-V patients from our prospective CNS vasculopathy registry.
Methods: We extracted CNS-V patients from our prospective CNS vasculopathy registry (n=201) from 2012-2019. Arterial involvement was assessed by digital subtraction angiography (DSA) or MR angiography (MRA). LMVV was defined as patients with cerebral vasculature indicating vasculitis in proximal or middle arterial segments. SVV was diagnosed with vessel involvements in only smaller distal branch or normal angiography. We compared clinical demographics, MRI findings including high-resolution vessel wall image (HR-VWI), and diagnostic accuracy for brain biopsy between two variants.
Results: We identified 34 cases who underwent cerebral vascular studies (DSA: n=26, MRA: n=32). Among them, 11 (32.4%) were LMVV and 23 (67.6%) were SVV based on angiographical findings. LMVV had more infarcts (LMVV: 100.0 % vs. SVV: 60.9%, P=0.017) and were more likely to have concentric vessel wall enhancement on HR-VWI (LMVV: 90.0% (9/10) vs. SVV: 7.1% (1/14), P< 0.001);summary in Table1.
By contrast, meningeal/parenchymal contrast enhancement lesion was more frequently observed in the SVV group (SVV: 87.0% vs. LMVV 45.5%, P=0.006) and the majority of SVV was diagnosed by brain biopsy (SVV: 78.3% vs. LMVV: 30.8%, P=0.022). The diagnostic accuracy of the brain biopsy was 100 % (18/18) in the SVV and 57.1% (4/7) in the LMVV, respectively (P=0.015);summary inTable 2.
Conclusion: Clinical and image characteristics of CNS-V seem to differ concerning the affected vessel size. LMVV is more likely to develop ischemic stroke and HR-VWI is useful for diagnosis of CNS-V with LMVV. Higher prevalence rate of mass lesion and leptomeningeal/parenchymal contrast enhancement lesion is associated with SVV; Brain biopsy is of high yield and thus should be considered in suspected CNS-V; higher yield of biopsy is associated with SVV variant but still positive in almost one third of LMVV variant
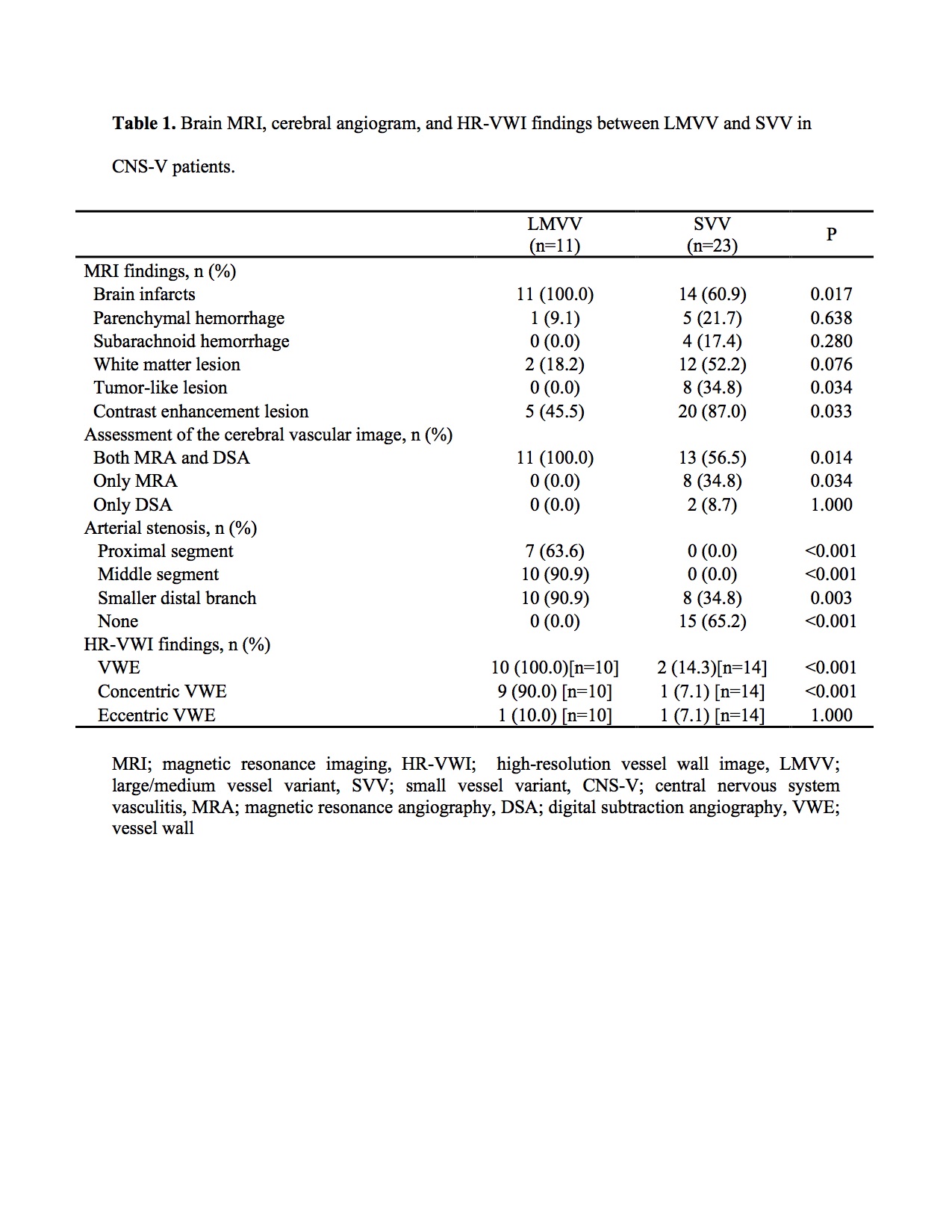 Brain MRI, cerebral angiogram, and HR-VWI findings between LMVV and SVV in CNS-V patients
Brain MRI, cerebral angiogram, and HR-VWI findings between LMVV and SVV in CNS-V patients
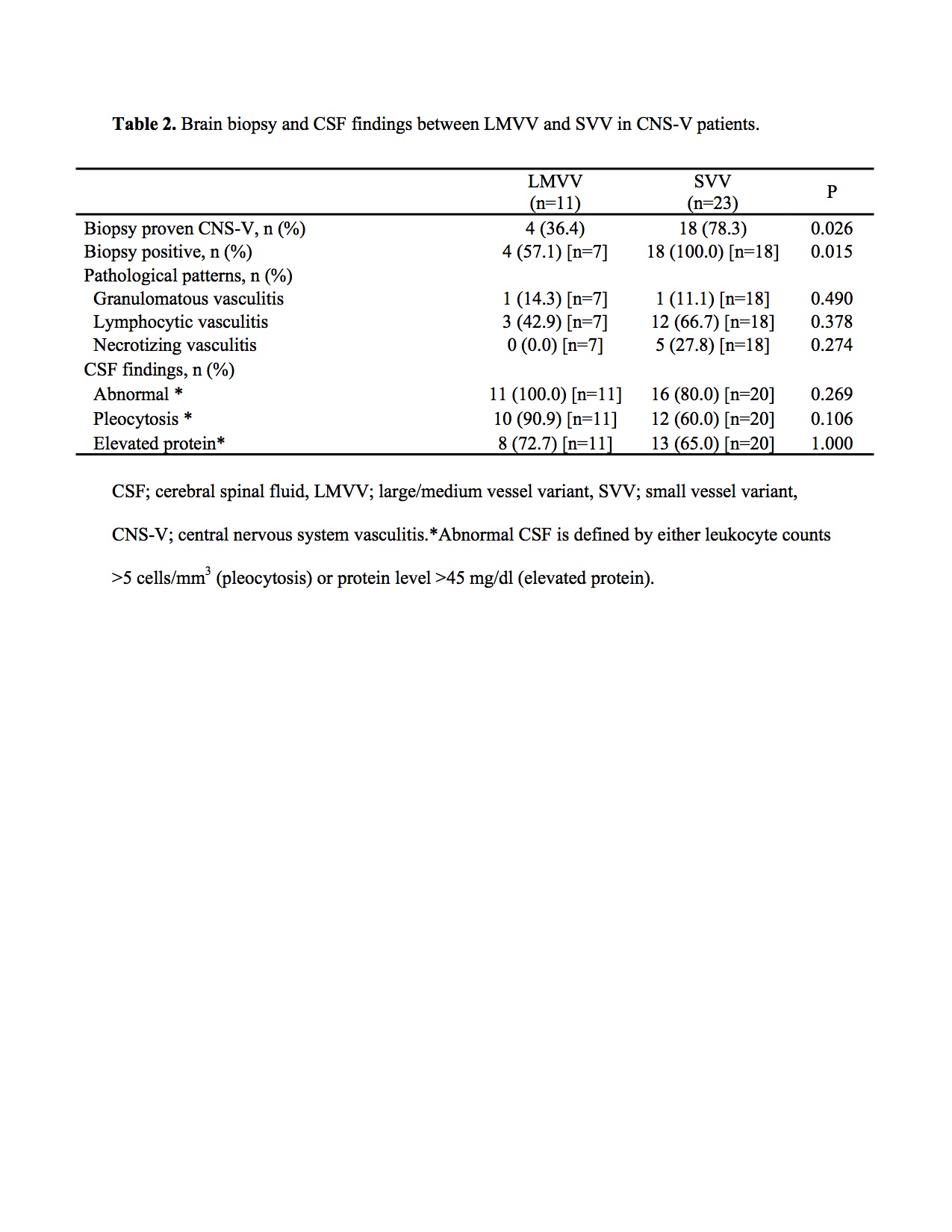 Brain biopsy and CSF findings between LMVV and SVV in CNS-V patients
Brain biopsy and CSF findings between LMVV and SVV in CNS-V patients
To cite this abstract in AMA style:
Shimoyama T, Uchino K, Calabrese L, Hajj-ali R. Clinical Characteristics, Brain MRI Findings, and Diagnostic Approach of the Central Nervous System Vasculitis by Affected Vessel Size [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/clinical-characteristics-brain-mri-findings-and-diagnostic-approach-of-the-central-nervous-system-vasculitis-by-affected-vessel-size/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-characteristics-brain-mri-findings-and-diagnostic-approach-of-the-central-nervous-system-vasculitis-by-affected-vessel-size/
