Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Aromatase inhibitors (AI) are frequently used in hormone receptor-positive breast cancer, which encompasses nearly 75% of all breast cancers. By preventing peripheral estrogen production, AIs magnify the effects of estrogen suppression during menopause causing accelerated bone loss at a rate 2-4 times higher than expected. Approximately 1 in 5 women treated with AI therapy will suffer from a fracture, increasing their risk of mortality. AI therapy is also used in men for the treatment of gynecomastia, but there is a lack of data regarding the effects of AIs on bone loss in men.
The American Society of Clinical Oncology recommends obtaining a baseline DXA in postmenopausal breast cancer survivors treated with an AI. Several studies have shown this screening is suboptimal but cost-effective in the U.S. The aim of this study was to assess our adherence to osteoporosis screening in patients on AI therapy and to understand factors that may influence screening.
Methods: In this retrospective cross-sectional study, clinic and hospital medical records were used to identify and analyze subjects on an aromatase inhibitor from January 2015 – January 2020. Descriptive and statistical analyses using Pearson’s Chi-Square were used to compare the characteristics of subjects who received DXA screening to those who did not.
Results: We identified 4,340 subjects on AI therapy from 2,248,780 charts available in the medical record system, giving AI therapy a prevalence of 0.19%. Of those, 3,797 (87.4%) were female and 549 (12.6%) were male. A DXA was ordered in 818 (19%) subjects and was not ordered in 3,522 (81%) subjects. Ninety-eight percent of subjects who had a DXA ordered were females [X2 (1, N=4340)=100.42, p< 0.01].
DXA screening was more likely to be ordered in subjects aged 65 years or older with a history of alcohol use [X2(2, N=4340)=54.94, p< 0.01], rheumatoid arthritis [X2(1, N=4340)=17.45, p< 0.01] , hypogonadism [X2(1, N=4340)=70.60, p< 0.01], and fragility fracture [X2(1, N=4340)=5.32, p< 0.025]. Among those who had DXA screening, the above factors were present in 51%, 5%, 2%, and 5%, respectively. Subjects with glucocorticoid [X2(1, N=4340)=30.93, p< 0.01], bisphosphonate [X2(1, N=4340)=7.79, p< 0.01], or vitamin D use [X2(1, N=4340)=35.92, p< 0.01] were also more likely to have DXA screening.
Conclusion: This investigation highlighted that osteoporosis screening for patients on AI therapy is low, despite the current guidelines. The osteoporosis risk factors associated with higher rates of screening were advanced age, alcohol use, rheumatoid arthritis, hypogonadism, and history of a fragility fracture. The rate of DXA screening was similar for patients with low BMI, tobacco use, type I diabetes mellitus, hyperthyroidism, liver disease, premature menopause, chronic malnutrition, and a family history of hip fracture. Males encompass nearly 13% of our population on AI therapy, and future studies are needed to understand the impact of AI treatment on bone health in men. More intense osteoporosis screening is needed for patients on AI therapy, especially for those with additional risk factors, and can be achieved through multidisciplinary collaboration.
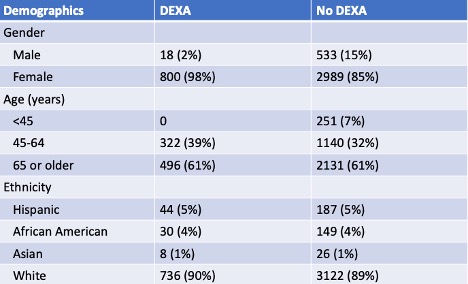 Table 1. Descriptive Analysis of Demographics
Table 1. Descriptive Analysis of Demographics
 Table 2. Descriptive Analysis of Osteoporosis (OP) Risk Factors
Table 2. Descriptive Analysis of Osteoporosis (OP) Risk Factors
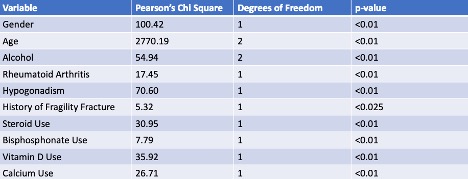 Table 3. Pearson’s Chi-Square Report of Statistically Significant Variables
Table 3. Pearson’s Chi-Square Report of Statistically Significant Variables
To cite this abstract in AMA style:
White M, Barre L. Aromatase Inhibitor-Associated Bone Loss: Screening and Prevention [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/aromatase-inhibitor-associated-bone-loss-screening-and-prevention/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/aromatase-inhibitor-associated-bone-loss-screening-and-prevention/
