Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: There is much controversy surrounding the loss of bone mass in patients with psoriasis arthritis (PsA). We wanted to evaluate the prevalence of osteoporosis (OP) and fracture in patients with PsA in the Swiss Clinical Quality Management (SCQM) cohort, a large national database of patients with inflammatory arthritis; to study different factors influencing bone health and the correlation between disease activity, treatment and occurrence of densitometric osteoporosis or fracture.
Methods: We analyzed all PsA-patients included in the cohort from 2006 to April 2019. We evaluated demographic and clinical data: age, gender, BMI, disease duration, smoking/alcohol habits, patient’s and physician’s global assessment, joint count, HAQ, medication and inflammatory activity measured by ESR, CRP, DAS 28 and DAPSA score. We compared patients with BMD measurement (DXA) with the group without DXA (nDXA). In DXA group we analyzed patients according to osteoporotic status and did subgroup analysis in premenopausal, menopausal women and men. We used STATA program vs 16, chi2-test, student’s t-test and simple and multiple regression models for statistics. Statistical significance was set up at p < 0.05.
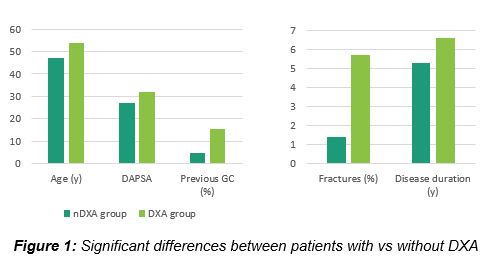
Results: Of the 2443 patients, 545 had a DXA. The age of scanned patients was 18-84 years. Only 295 BMD data were available for analysis. DXA patients were 6.4 years older (54.2±11,1 vs 47.8±12.4 years, p< 0.001), and were more female (67% vs 43%). Duration of the disease was longer (6.6±8.3 vs 5.3±7.1 y, p< 0.001) in the DXA group. DAS28-CRP and DAS28-ESR were higher in DXA group (3,1 ± 1,2 vs 2,9 ± 1,1, p< 0,04 and 3,2 ± 1,4 vs 3 ± 1,3, p< 0,002, respectively), as was the DAPSA score (32 ± 30 vs 27 ± 20 p< 0.04). Patients in DXA group were more exposed to prednisone and conventional DMARDs (15.4% vs 4.7%, p< 0.001 and 51.7% vs 43%, p< 0.01 respectively). There were more fractures in the DXA- than in nDXA-group (5.7% vs 1.4%, P< 0.001) (Figure 1).
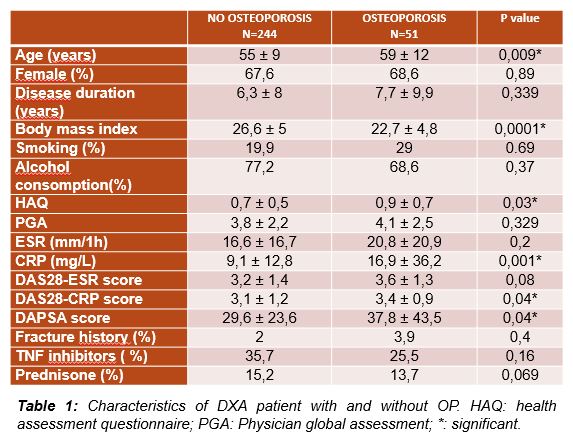
In the DXA group 18.4% patients had OP and 50.2% osteopenia. Patient characteristics are shown in Table 1. We confirmed a positive correlation between femoral and lumbar T-score and BMI, and negative correlation between age and femoral T-score. Disease duration was inversely correlated with femoral, but not lumbar T-score. Interestingly, other variables, including disease activity, showed no correlation with T-score, but OP patients had higher disease activity.
Subgroup analysis (Figure 2) showed higher OP prevalence in postmenopausal women (22,6%) vs in men (16.8%) or premenopausal women (10.7%) in concordance with the fracture rate (8.3% vs 6.3% vs 3.9%). T-score was lower and the disease activity was higher in postmenopausal women compared to the others groups.
Conclusion: Our data suggest that Swiss clinician are aware of risk of poor bone-health in PsA patients and perform DXA in this population even in younger patients and in men. Interestingly, we describe that the patients with OP had higher disease activity and poorer functional status than patients without OP.
Longitudinal studies are needed to evaluate bone quality, fractures, and relationship between bone health in PsA and disease associated factors. They should integrate parameters of bone turnover and use an appropriate control group.
To cite this abstract in AMA style:
Dan D, Ibrahimy Y, Aubry-Rozier B, Aeberli D. Bone Health in Patients with Psoriatic Arthritis in the National Swiss Cohort: A Cross-sectional Study [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/bone-health-in-patients-with-psoriatic-arthritis-in-the-national-swiss-cohort-a-cross-sectional-study/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/bone-health-in-patients-with-psoriatic-arthritis-in-the-national-swiss-cohort-a-cross-sectional-study/