Session Information
Session Type: ACR Abstract Session
Session Time: 11:00AM-12:30PM
Background/Purpose: Cutaneous lupus erythematosus (CLE) is an autoimmune disease with various subsets and clinical manifestations. T lymphocytes are the predominant cell type found in lesional skin, but plasmacytoid dendritic cells (pDCs) and myeloid dendritic cells (mDCs) also play an important role in the pathogenesis. Oral antimalarials, including hydroxychloroquine (HCQ) and quinacrine (QC) are first-line systemic therapy for all CLE sub-types. Although HCQ is effective in approximately 50% of patients, some patients still do not respond to antimalarials. Some of these patients benefit from additional QC, but there is a subset of patients who remain refractory to both antimalarials. Refractoriness poses a huge challenge as patients continue to have active disease despite antimalarial therapy. To better understand reasons for refractoriness in CLE, we investigated the immunologic characteristics of patients who responded to antimalarials versus those who did not.
Methods: One hundred fifteen patients with a diagnosis of CLE were recruited from the Autoimmune Skin Disease Center at the Hospital of the University of Pennsylvania. Sixty-five were well-characterized in terms of response to treatment as (i) HCQ-responders (n=22), (ii) HCQ+QC-responders (n=24), or (iii) HCQ+QC-nonresponders (n=19). Lesional skin was biopsied before starting treatment with antimalarials. We defined treatment failure to HCQ as continued skin activity requiring a second intervention after at least 2 months of HCQ therapy. Immunohistochemistry was used to characterize the inflammatory cells and cytokine expression in lesional skin biopsies from patients. Total RNA was extracted from these biopsies to analyze specific gene signatures. The patient’s CLASI score – a measure of disease activity – at the time of the biopsy was also determined.
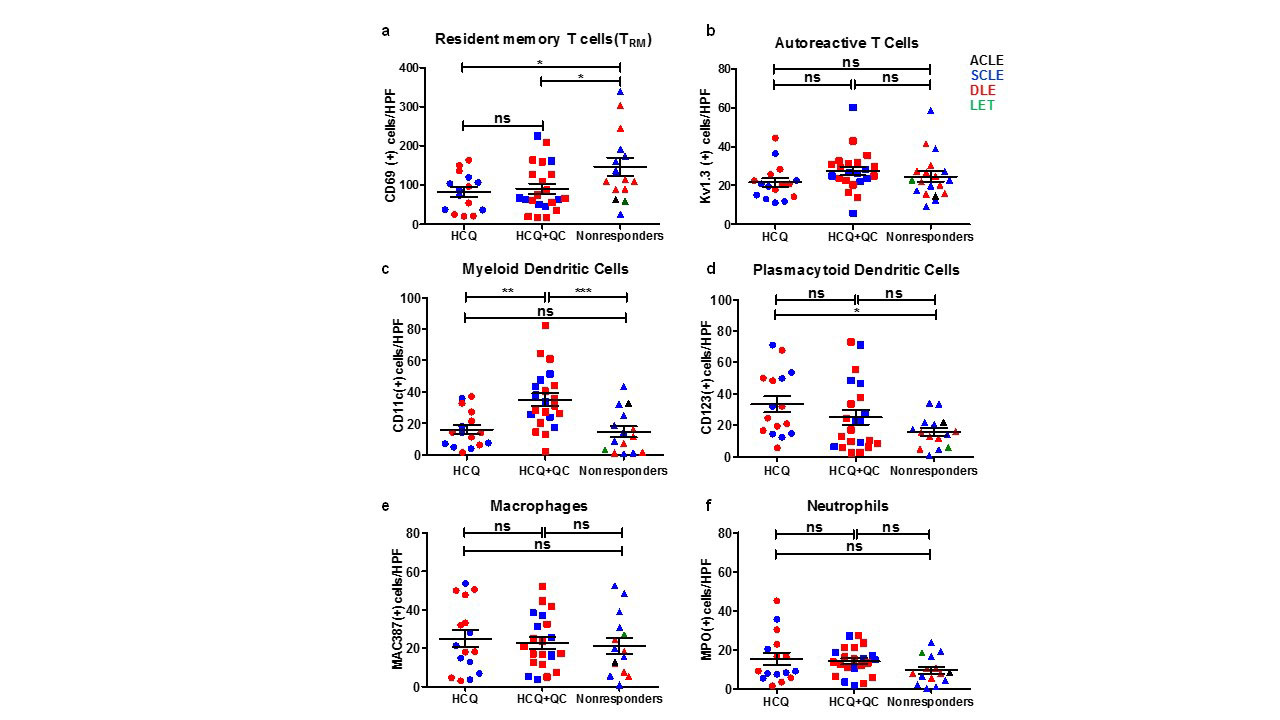
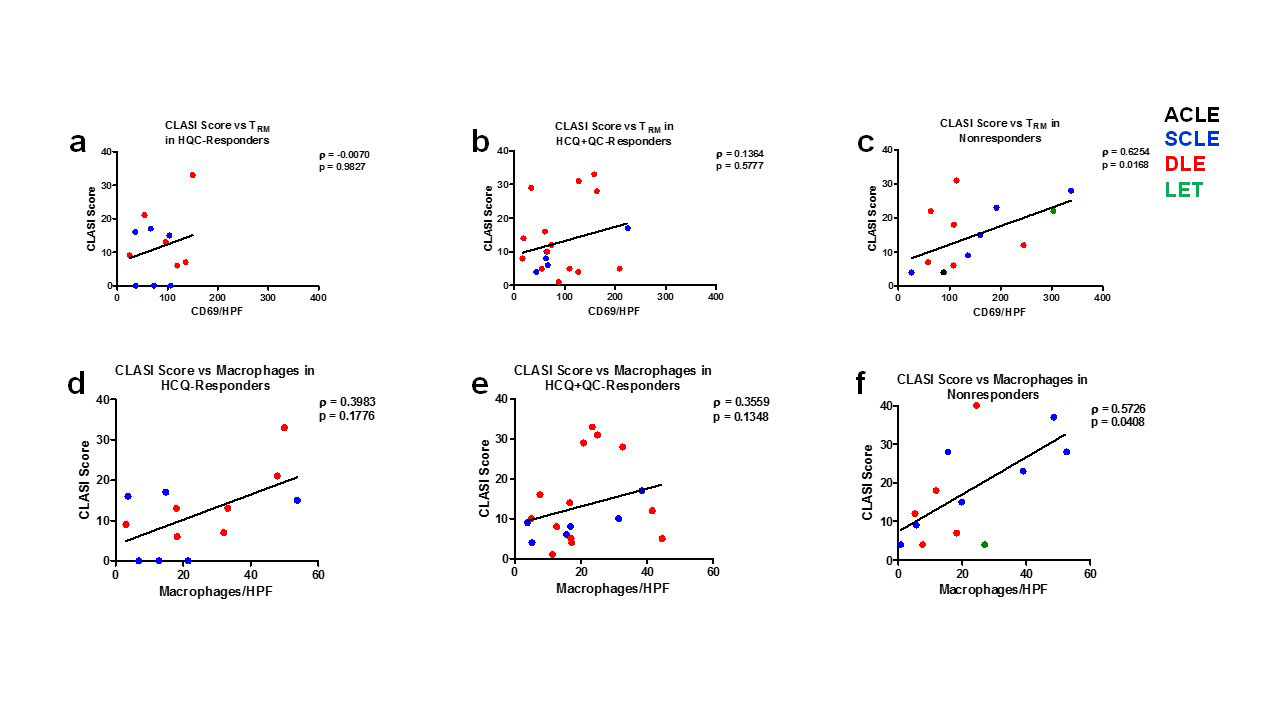
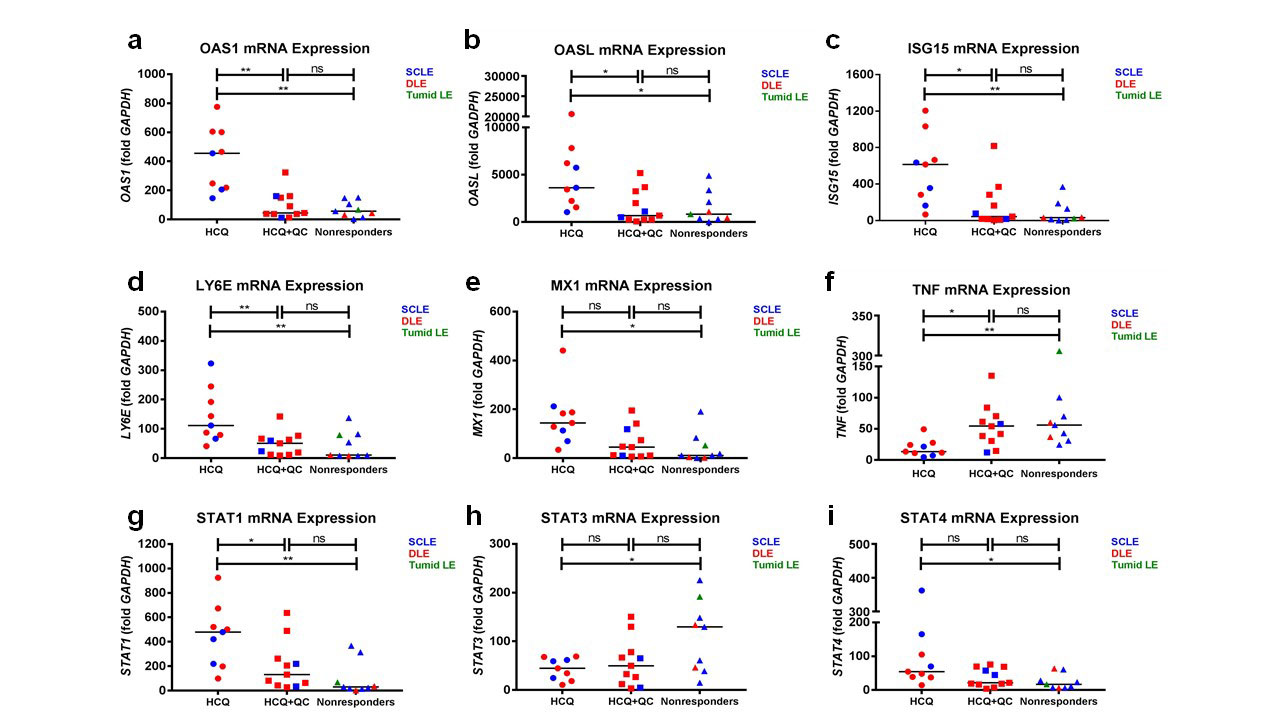
Results: Immunohistochemistry showed that CD69+ tissue-resident memory T (TRM) cells were significantly higher in HCQ+QC-nonresponders compared to HCQ- and HCQ+QC-responders. mDCs were significantly higher in HCQ+QC-responders compared to HCQ- and HCQ+QC-nonresponders. There were significantly higher pDCs in the HCQ-responders compared to the nonresponders. There was no significant difference in the number of autoreactive T cells, macrophages, and neutrophils among the three groups (Figure 1). The HCQ+QC-nonresponder group was distinct from the other groups in that their CLASI scores correlated positively with the number of TRM cells (r=0.6254, p=0.017) and macrophages (r=0.5726, p=0.041) (Figure 2). mRNA expression demonstrated high STAT3 expression in HCQ+QC-nonresponders (Figure 3). There was a significantly higher percentage of area stained for IL-17 in the HCQ+QC-responders compared to HCQ-responders and HCQ+QC-nonresponders while IL-22 expression was not significantly different between groups.
Conclusion: An increased number of CD69+ TRM cells and correlation between CD69+TRM cells and macrophages with CLASI scores in the HCQ+QC-nonresponders, a finding not seen in either HCQ or HCQ+QC-responders, may indicate that CD69+ TRM cells and macrophages are involved in antimalarial-refractory skin disease.
The nonresponders and HCQ+QC-responders had a similar expression profile for all analyzed genes.
To cite this abstract in AMA style:
Zeidi M, Chen K, Desai K, Kim H, Chakka S, Lim R, Werth V. Increased CD69+ Tissue-resident Memory T (TRM) Cells and STAT3 Expression in Cutaneous Lupus Erythematosus Patients Recalcitrant to Antimalarials [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/increased-cd69-tissue-resident-memory-t-trm-cells-and-stat3-expression-in-cutaneous-lupus-erythematosus-patients-recalcitrant-to-antimalarials/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/increased-cd69-tissue-resident-memory-t-trm-cells-and-stat3-expression-in-cutaneous-lupus-erythematosus-patients-recalcitrant-to-antimalarials/