Session Information
Date: Tuesday, November 12, 2019
Title: Pediatric Rheumatology – ePoster III: Systemic JIA, Fever, & Vasculitis
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: The transition from pediatric to adult-oriented health care represents a vulnerable period for young adults with chronic rheumatic diseases. In spite of this, a 2010 study of Childhood Arthritis and Rheumatology Research Alliance (CARRA) rheumatologists showed that less than 10% were familiar with existing transition guidelines. Since then, new health care transition guidelines and an ACR transition toolkit have been disseminated. We resurveyed CARRA members to assess the impact of new guidelines and tools on transition practices and explored predictors of transition practices.
Methods: An online survey on health care transition was emailed to CARRA providers in April 2018. Pediatric rheumatology physicians and fellows in the United States (U.S.) or Canada were included in analysis. Univariate comparisons and multivariate linear and logistic regression were performed to identify factors that predict age of transfer and transition practices, including self-assessed performance on Got Transition’s Current Assessment of Health Care Transition Activities (CAHCTA), which measures the level of health care transition support provided by a practice, with scores ranging from 6 (basic) to 24 (comprehensive).
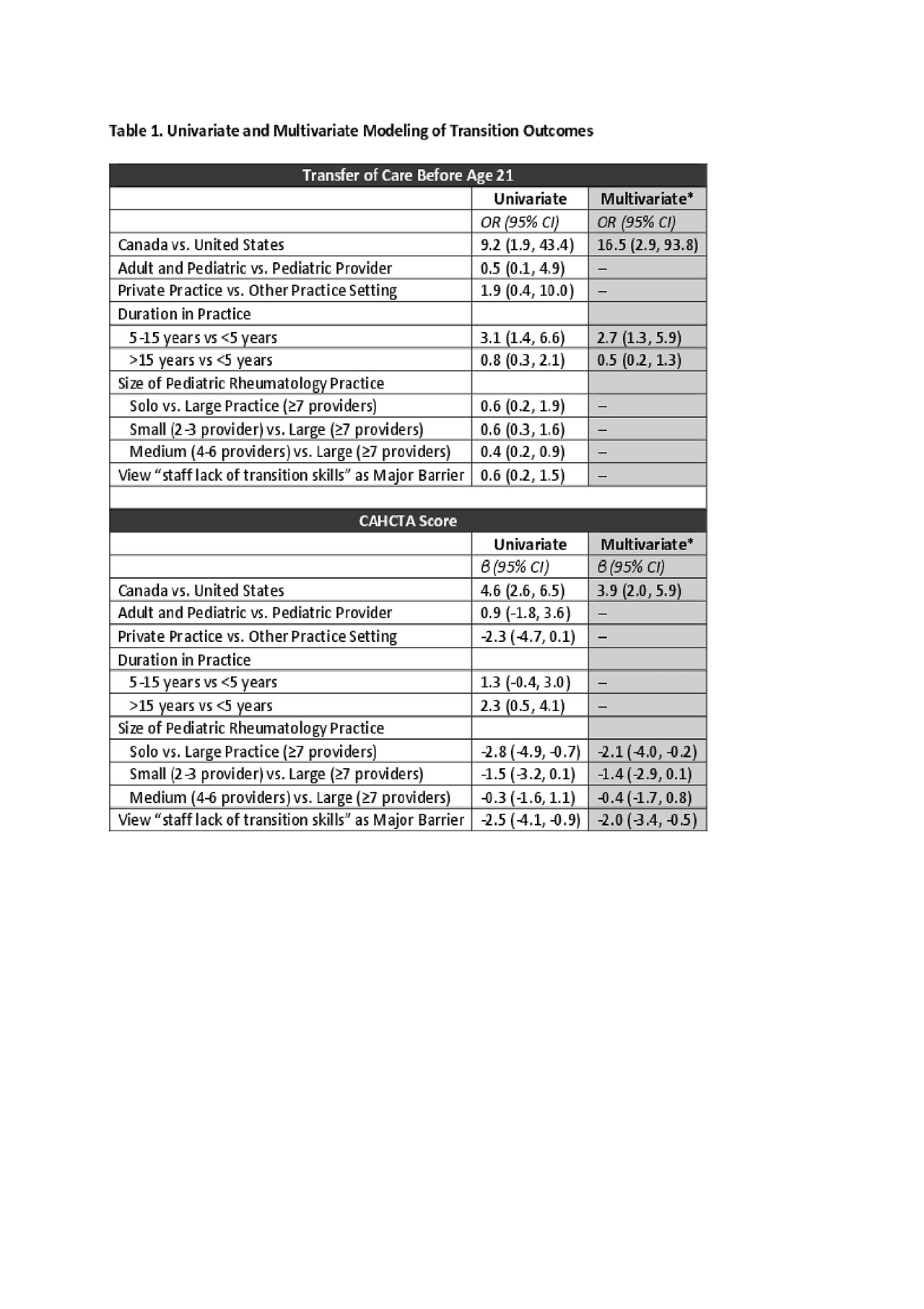
Results: The response rate was 212/396 (54%), of which 192 responses were analyzed: 147 pediatric rheumatologists, 8 dual-boarded adult/pediatric rheumatologists, and 37 fellows, inclusive of 180 U.S. and 12 Canadian providers (from 4 academic institutions). Table 1 shows unadjusted, univariate statistics alongside multivariate modeling for transfer age and CAHCTA score. In multivariate analysis, providers who transfer patients prior to age 21 are more likely to practice in Canada (OR=16.6, 95% CI: 3.0-92.4) and to have been in practice for 5-15 years (OR=2.7, 95% CI: 1.3-5.6). Whereas 92% of Canadian providers routinely ask parents leave the room for at least part of the visit before patients reach the age of 18, only 41% of U.S. respondents do so (p=0.001). Similarly, 56% of private practice pediatric rheumatologists use an adult model of care, compared to only 20% in other practice settings (p=0.03). Finally, Canadian pediatric rheumatologists have a significantly higher mean CAHCTA score (15.0 v 10.3; p< 0.0001), whereas providers believing pediatric staff lack skills in transition support have lower scores (8.7 vs 11.0; p=.003).
Conclusion: This survey highlights clinic staff training in transitional care skills as a potential avenue to enhance health care transition support in pediatric rheumatology. In addition, this survey underscores ways in which transition support services are more established in Canada, given stricter mandates to transfer patients at age 18 and the subsequent development of national strategies to support young adults. Canadian CARRA members’ experiences with transitional support services will contribute to CARRA’s new Transition Learning Collaborative, developed to facilitate dissemination and implementation of transition programs and services in a way that addresses the heterogeneous landscape of health care transition.
To cite this abstract in AMA style:
Sadun R, Eudy A, Chiraseveenuprapund P, Edens C, Hersh A, Johnson K, Lawson E. Predictors of Health Care Transition Practices Among North American Pediatric Rheumatology Providers [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/predictors-of-health-care-transition-practices-among-north-american-pediatric-rheumatology-providers/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/predictors-of-health-care-transition-practices-among-north-american-pediatric-rheumatology-providers/