Session Information
Date: Tuesday, November 12, 2019
Title: Systemic Sclerosis & Related Disorders – Clinical Poster III
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Interstitial lung disease (ILD) and pulmonary arterial hypertension negatively impact on Systemic sclerosis (SSc) prognosis. Chest computed tomography (CT) is the gold standard in assessing ILD and helps in evaluating associated vascular involvement. However, CT scans qualitative analysis is limited by low reproducibility and time constraints. Recently developed quantitative techniques may overcome these limitations. We aimed at evaluating parenchymal and vascular features in SSc-ILD by using quantitative analysis (QA) of CT scans and test correlation with clinical-functional data.
Methods: We analyzed chest CT scans in SSc patients performed with spirometric gating at TLC. A computational platform for texture analysis of ILD patterns (CALIPER), through Imbio LTA Launchpad, quantified the extent of normal pattern (NP%), ground glass opacities (GG%), reticulation (RET%), and honeycombing (HC%) [1]. An automated vessels segmentation was performed using a software program developed by the Ludwig Boltzmann Institute for Lung Vascular Research [2], calculating total, arterial, and venous vascular volumes (TV, AV, VV), and relative volumes (TV%, AV%, VV%). Clinical, lung functional and diffusion data, as well as disability indexes were also collected.
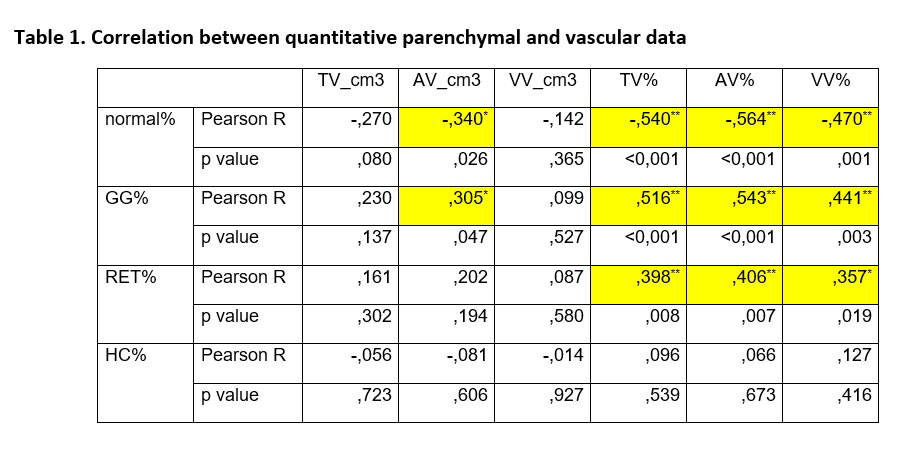
Results: 44 patients/CT scans were eligible (89% female, 42% diffuse, 7% PAH) for both software analysis. CALIPER showed GG% as the most frequent radiological pattern (median 2.7%, 0.2-7.6 IQR), with positive correlation with mRSS (r=0.363, p=0.016) and increasing NYHA class (r=0.306, p=0.037), while negative correlation with FVC (r=-0.371, p=0.009) and TLC (r=-0.356, p=0.024). Similarly, RET% showed positive correlation with mRSS (r=0.491, p=0.001) and negative correlation with desaturation on 6 minutes walking test (r=-0.433, p=0.017). On the vascular analysis, TV% had positive correlation with increasing NYHA class (r=0.319, p=0.048), difficulty increase in walking domains of HAQ-DI (r=0.607, p=0.002) and Dlco/AV (r=0.414, p=0.007), while negative correlation with FVC (r=-0.449, p=0.003) and TLC (r=-0.496, p=0.003), with similar significant correlations replicated for AV%. When testing parenchymal with vascular data (Table 1), higher GG% and RET% correlated with higher vascular relative volumes. In addition, GG% correlated with AV. Conversely, increasing NP% was associated to a decrease in AV and in all vascular relative volumes.
Conclusion: This is the first study that shows a direct link between ILD and increase in lung vascular volume in SSc patients. Different hypothesis could be postulated, such as a reduction in pulmonary volume due to fibrosis, an increase in absolute vascular volumes as a phenomenon of neo-angiogenesis secondary to fibrosis, or a para-physiological mechanism of redistribution of blood flow in lung areas less involved by ILD. Further studies on lung vessel quantification and distribution are ongoing.
To cite this abstract in AMA style:
Bruni C, Occhipinti M, Camiciottoli G, Bartolucci M, Pienn M, Lepri G, Fabbrizzi A, Tottoli A, Ciardi G, Giuggioli D, Cuomo G, Masini F, Olschewski A, Lavorini F, Colagrande S, Matucci-Cerinic M. Relationship Between Parenchymal and Vascular Features in Systemic Sclerosis-Interstitial Lung Disease: Results from Quantitative Analysis of Chest Computed Tomography [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/relationship-between-parenchymal-and-vascular-features-in-systemic-sclerosis-interstitial-lung-disease-results-from-quantitative-analysis-of-chest-computed-tomography/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/relationship-between-parenchymal-and-vascular-features-in-systemic-sclerosis-interstitial-lung-disease-results-from-quantitative-analysis-of-chest-computed-tomography/