Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Although treatment of inflammatory arthritis (IA) has improved, opioid use among patients remains common. A study from Finland showed increases in opioid use leading up to a diagnosis of IA, then a decrease after diagnosis, and that opioid use in axial spondyloarthritis was higher than in other IAs.1 In a study of patients with AS, 44% of patients were using opioids, and 26% of these patients were using only opioids.2 The timing of opioid use surrounding IA diagnosis in the USA is not known. The objective of this study was to describe opioid use in the year preceding and following diagnosis of AS, RA, and PsA.
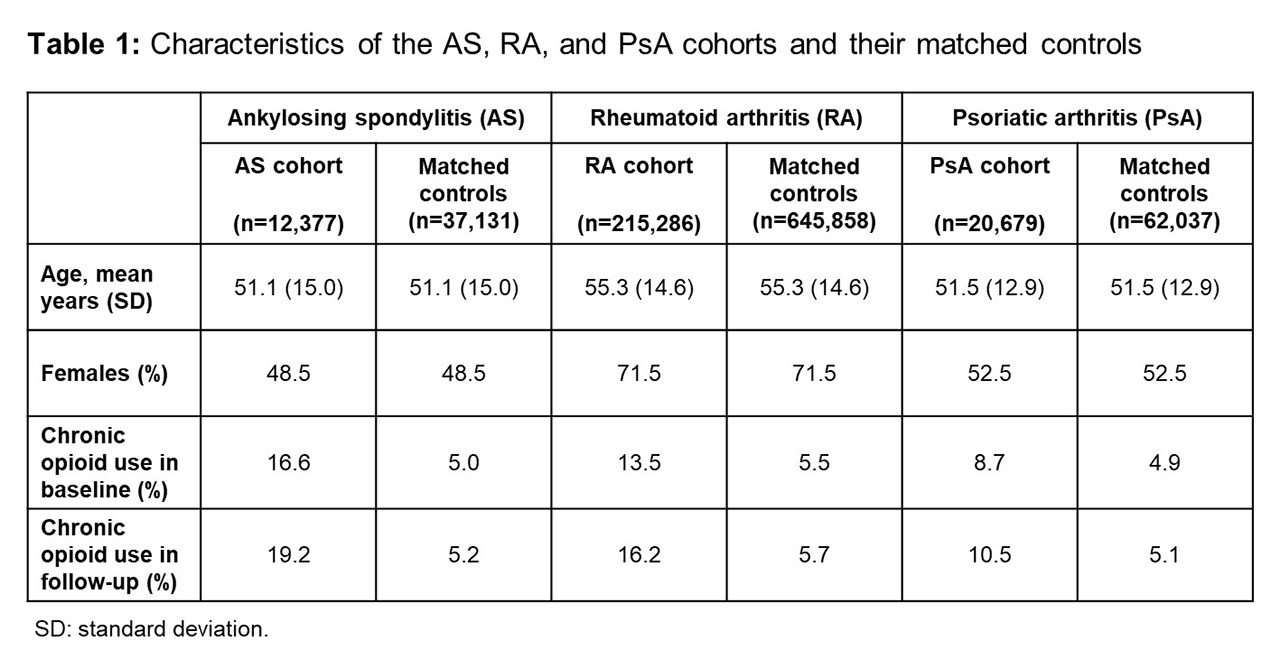
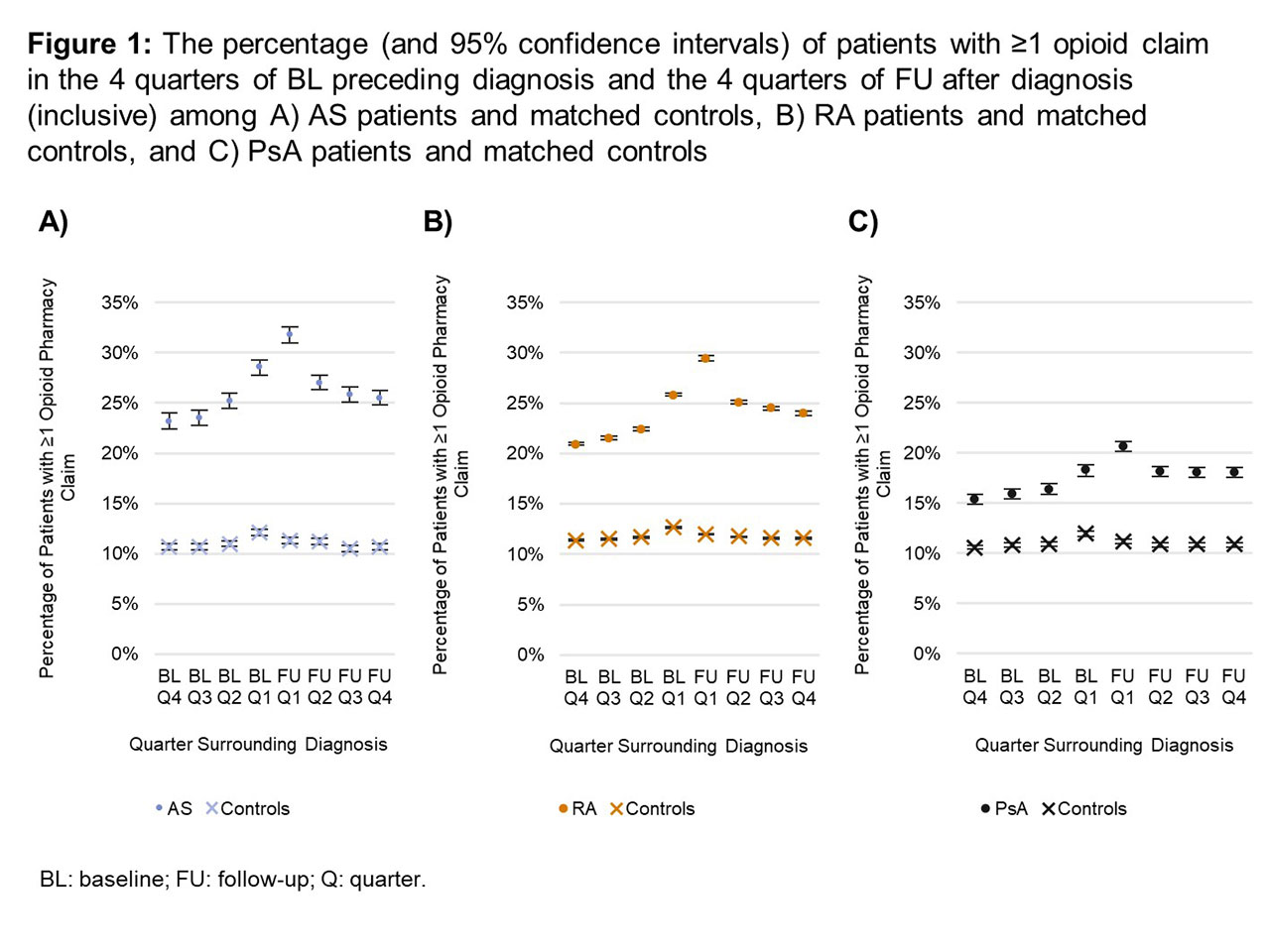
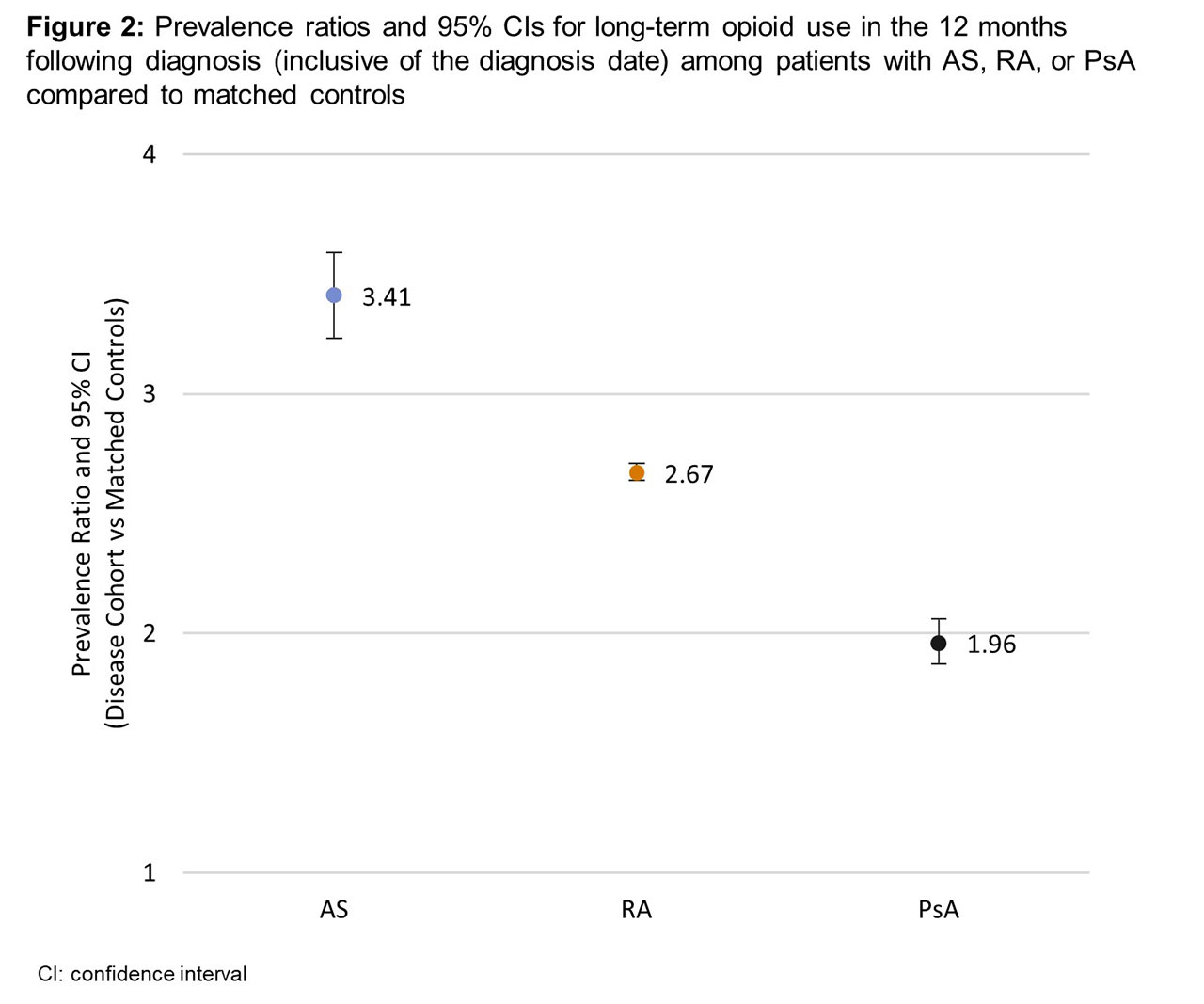
Methods: This retrospective observational study analyzed USA commercial claims data (IBM® MarketScan®) from patients with an International Classification of Diseases (ICD) 9/10 code for AS, RA, or PsA (index date) between 2010–2017. Three controls, matched on year, age, sex, region, and insurance plan type, were selected for each disease case. Opioid pharmacy claims were examined in a 12-month baseline (BL) and 12-month follow-up (FU) period after index date with further division into 3-month periods. Chronic opioid use was defined as ≥90 cumulative days’ supply in a 12-month period and was assessed separately in BL and FU. Long-term use was defined as ≥1 opioid claim in ≥3 of 4 quarters in FU. Prevalence ratios for long-term opioid use in the disease vs matched control cohorts were calculated for FU.
Results: The study included 12,377 AS, 215,286 RA, and 20,679 PsA patients (Table). In all 3 cohorts, prevalence of opioid exposure was highest in the quarter following (inclusive of) diagnosis, and prevalence of use was higher in all disease vs matched control cohorts for each quarter (Figure 1). Compared to matched controls, prevalence of chronic opioid use was higher in disease cohorts in BL and FU (Table), and prevalence of long-term use in FU was also higher (Figure 2).
Conclusion: Opioid use is common among patients with IA in both the year preceding and the year following diagnosis, peaking at the time of diagnosis. For all IAs, prevalence of opioid claims and long-term opioid use were higher than in matched controls. Although patterns in these data are similar to those seen in Finland, the overall prevalence of any opioid use (in cases and controls) was higher in the USA. The prevalence of long-term opioid use was highest in AS patients compared to matched controls and highest among the 3 IAs, similar to the finding in Finland. The prevalence of opioid use in IA suggests the presence of uncontrolled pain in the period surrounding diagnosis. Given the ineffectiveness of opioids to address the underlying cause of IA, more comprehensive or appropriate treatments such as DMARDs and/or biologics to address the underlying disease should be considered, in accordance with relevant guidelines.
References:
1. Muilu P. Ann Rheum Dis 2018;77:A156; 2. Sloan V. J Rheum 2019; doi: 10.3899/jrheum.180972.
To cite this abstract in AMA style:
Sheahan A, Sloan V, Stark J, Suruki R. Opioid Use Surrounding Diagnosis of Inflammatory Arthritis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/opioid-use-surrounding-diagnosis-of-inflammatory-arthritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/opioid-use-surrounding-diagnosis-of-inflammatory-arthritis/