Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
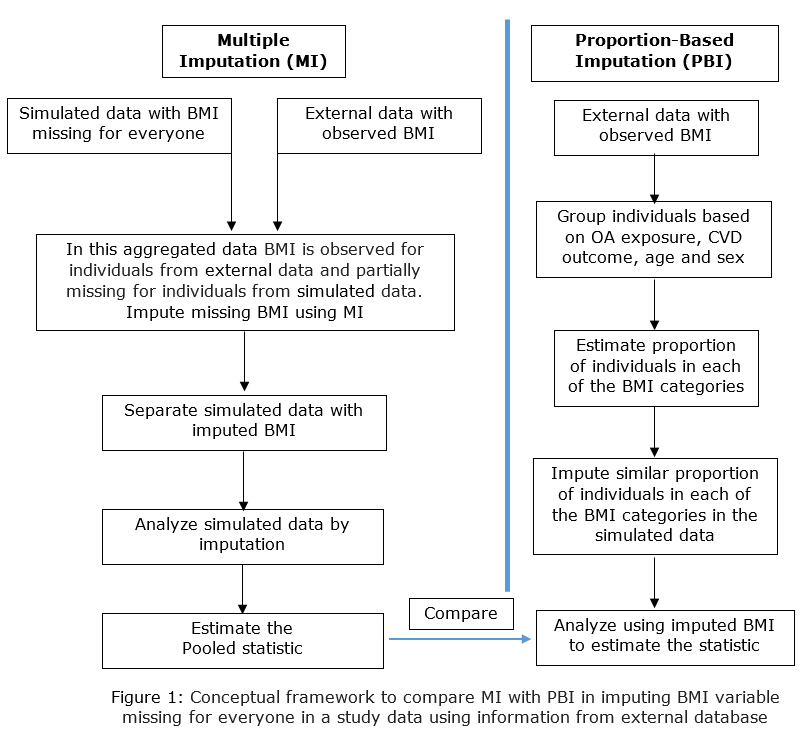
Background/Purpose: BMI is a well-known confounding factor in the association between osteoarthritis (OA) and cardiovascular diseases (CVD). However, BMI is not usually recorded in administrative databases. When BMI is imputed using the proportion-based imputation (PBI) method, a BMI category is assigned to an individual according to the proportions observed in external data based on a set of pre-defined variables (1). Alternatively, standard Multiple Imputation (MI) methods can also be employed in the same situations. We investigated the OA-CVD relationship as a demonstration to compare MI with PBI (figure 1). We hypothesized that BMI imputed using MI will minimize potential bias in the OA-CVD association compared to BMI categories imputed using PBI.
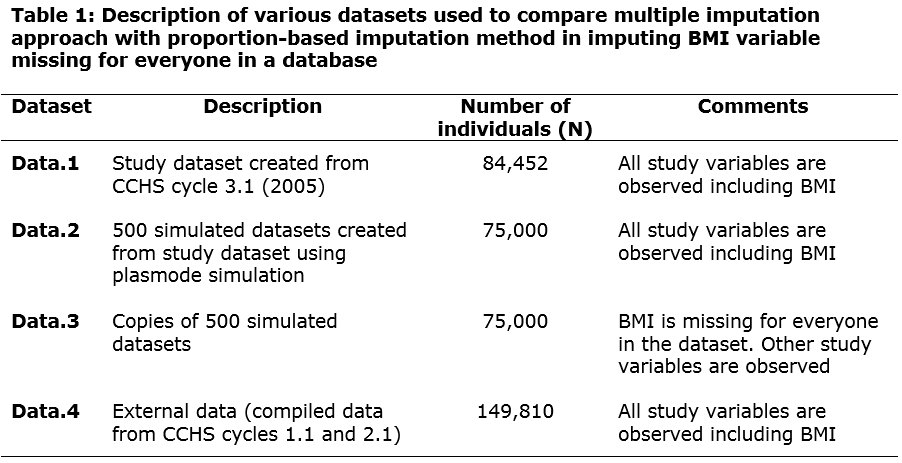
Methods: In this plasmode simulation study 500 simulated datasets were created using publicly available data from the Canadian Community Health Survey (CCHS) cycle 3.1. BMI was set missing for everyone in the simulated data. This mimics administrative data in which BMI is not recorded and missing for everyone in the database. A large dataset compiled from CCHS cycles 1.1 and 2.1 served as the external data in which BMI was observed for everyone. Table 1 summarizes the databases accessed. BMI missing in copies of simulated data was imputed using MI (with a number of imputations = 5) and PBI accessing observed BMI information in external data. To evaluate the performance of imputation methods, the distribution of the BMI variable and the adjusted odds ratio (aOR) estimated from the multivariable logistic regression model were compared. In this model, CVD outcome was regressed on OA exposure adjusting for age, sex, physical activity index, level of education, household income level, smoking status, diabetes, hypertension and BMI category. After analyzing the imputed datasets, the proportion of individuals in each of the four BMI categories and the ORs were averaged from the 500 simulated datasets. The 95% confidence interval (CI) of the averaged OR was calculated by the percentile method.
Results: Compared to PBI, MI produced proportions of individuals closer to the known proportions across the BMI categories except for the overweight category (Table 2). Considering the known aOR of 1.59 (1.36, 1.82), BMI imputed using MI introduced less bias in OA-CVD association compared to PBI, the aOR was 1.62 (1.39, 1.86) and 1.66 (1.41, 1.90), respectively.
Conclusion: This is the first study to compare MI with PBI in the context of imputing BMI information that is not recorded at the database level. MI was superior to imputation method based on population-level proportions in imputing BMI missing for everyone in the simulated datasets. The generalizability of these methodological results will become more evident as more similar studies are undertaken in a variety of settings.
Reference
1. Rahman MM, Kopec JA, Anis AH, Cibere J, Goldsmith CH. Risk of Cardiovascular Disease in Patients With Osteoarthritis: A Prospective Longitudinal Study: Cardiovascular Disease in Osteoarthritis Patients. Arthritis Care Res. 2013 Dec;65(12):1951–8.
To cite this abstract in AMA style:
Atiquzzaman M, Karim M, Kopec J, Wong H, De Vera M, Anis A. Using External Data to Estimate Omitted Variables in Observational Data: A Plasmode Simulation Study Investigating the Relationship Between Osteoarthritis and Cardiovascular Diseases to Compare Alternative Approaches in Imputing the Body Mass Index Variable [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/using-external-data-to-estimate-omitted-variables-in-observational-data-a-plasmode-simulation-study-investigating-the-relationship-between-osteoarthritis-and-cardiovascular-diseases-to-compare-altern/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/using-external-data-to-estimate-omitted-variables-in-observational-data-a-plasmode-simulation-study-investigating-the-relationship-between-osteoarthritis-and-cardiovascular-diseases-to-compare-altern/