Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Delays in treatment for inflammatory arthritis (IA) are associated with unfavorable outcomes, including impaired quality of life, irreversible joint damage, and disability. Our objective of this study was to characterize treatment initiation patterns in Veterans with newly diagnosed rheumatoid arthritis (RA), psoriatic arthritis (PsA) or ankylosing spondylitis (AS).
Methods: International Classification of Diseases codes and natural language processing were used to identify incident cases of RA, PsA, or AS, between January 1, 2007 and December 31, 2015, in patients enrolled in the Veteran Health Administration. Patterns of treatment initiation and non-treatment with disease modifying anti-rheumatic drugs (DMARDs) were assessed in the 12-month follow-up period after the incident diagnosis (Figure 1). Confidence intervals were used to statistically evaluate differences between comparison groups.
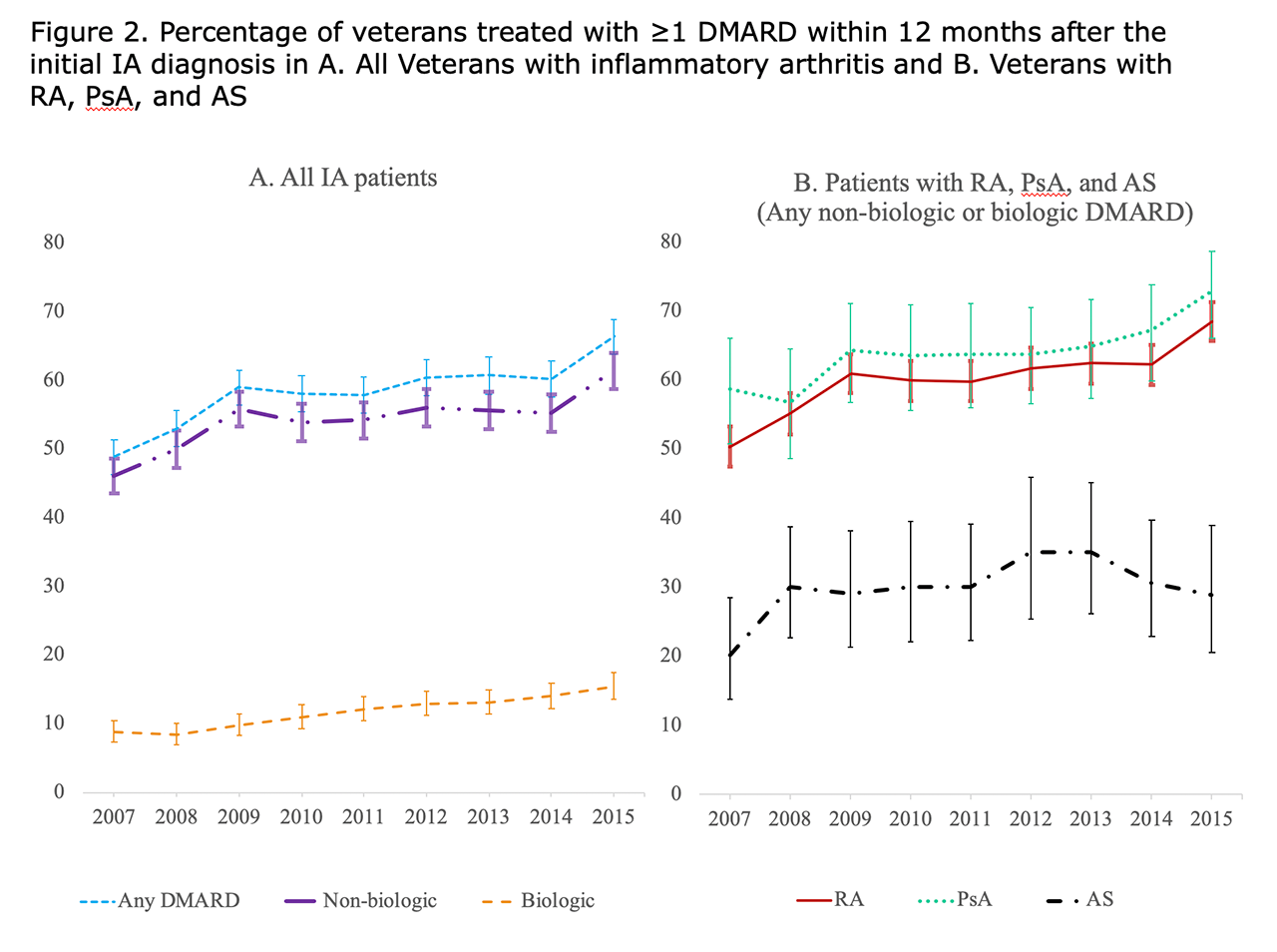
Results: The population consisted of 12,118 IA patients (9,711 RA, 1,472 PsA, 935 AS), with 91.3% males and a mean age of 63.7 (Table 1). The percentage of Veterans treated with ≥1 DMARD during the 12-month follow-up period increased from 48.8% in 2007 to 66.4% in 2015. Amongst Veterans diagnosed with IA in 2015, DMARD treatment was more common for PsA patients (72.9%) and RA patients (68.6%) than AS patients (28.9%). The mean time to the initial DMARD after diagnosis did not change over the observation period (35.5 days for RA, 43.9 days for PsA, 59.5 days for AS). In Veterans diagnosed with IA in 2015, a DMARD was dispensed ≤30 days after diagnosis in 45.8%, 31-90 days in 10.1%, and 91- 365 days for 10.5%; the remaining 33.6% were not treated with a DMARD within the 365-day follow-up period (Figure 2). Rheumatology specialty care was accessed by 87.4% of Veterans treated with a non-biologic DMARD and 92.2% treated with a biologic DMARD, in patients diagnosed in 2015.
Conclusion: DMARD treatment rates during the initial 12 months after diagnosis increased between 2007 and 2015, but non-treatment remained common, particularly in Veterans with AS. Time to treatment after the initial IA diagnosis did not change throughout the study period, and DMARDs were dispensed within 30 days of diagnosis for most Veterans who were treated within the 1-year follow-up period. DMARD treatment was uncommon in patients without rheumatology specialty care.
To cite this abstract in AMA style:
Overbury R, Pei S, Penmetsa G, Sauer B, Patil V, Walker J, Clewell J, Douglas K, Clegg D, Cannon G, Halwani A, Walsh J. Treatment Patterns with Disease Modifying Anti-rheumatic Drugs in United States Veterans with Newly Diagnosed Rheumatoid Arthritis, Psoriatic Arthritis, or Ankylosing Spondylitis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/treatment-patterns-with-disease-modifying-anti-rheumatic-drugs-in-united-states-veterans-with-newly-diagnosed-rheumatoid-arthritis-psoriatic-arthritis-or-ankylosing-spondylitis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/treatment-patterns-with-disease-modifying-anti-rheumatic-drugs-in-united-states-veterans-with-newly-diagnosed-rheumatoid-arthritis-psoriatic-arthritis-or-ankylosing-spondylitis/