Session Information
Date: Tuesday, November 12, 2019
Title: RA – Diagnosis, Manifestations, & Outcomes Poster III: Comorbidities
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: A wide spectrum of interstitial lung abnormalities (ILA) occurs in patients with rheumatoid arthritis (RA). This study characterized ILA in large single-center cohort, including identification of risk factors and parameters that may influence ILA´s progression.
Methods: All clinically-indicated computed tomography (CT) chest scans performed in adult RA patients from 2014-16 were evaluated for the presence of ILA using a sequential reading method. ILA were defined as nondependent changes affecting more than 5% of any lung zone and included nondependent ground-glass or reticular opacities, diffuse centrilobular nodularity, nonemphysematous cysts, honeycombing or traction bronchiectasis. Scans were classified as (a) no ILA, (b) indeterminate (focal alterations with less than 5% involvement of the lung) or (c) ILA; ILA were further subdivided into subpleural, centrilobular, mixed, and extensive distributions.The progression of ILA was determined visually and subsequently quantified by two independent observers blinded to clinical information. Univariate analyses were conducted with Fisher exact test and two-tailed t-tests or Wilcoxon rank-sum tests where appropriate. For multivariate analyses, unadjusted and adjusted logistic regression models were used to assess the strength of the association between RA-ILA and variables of interest. P-values < 0.05 were considered statistically significant.
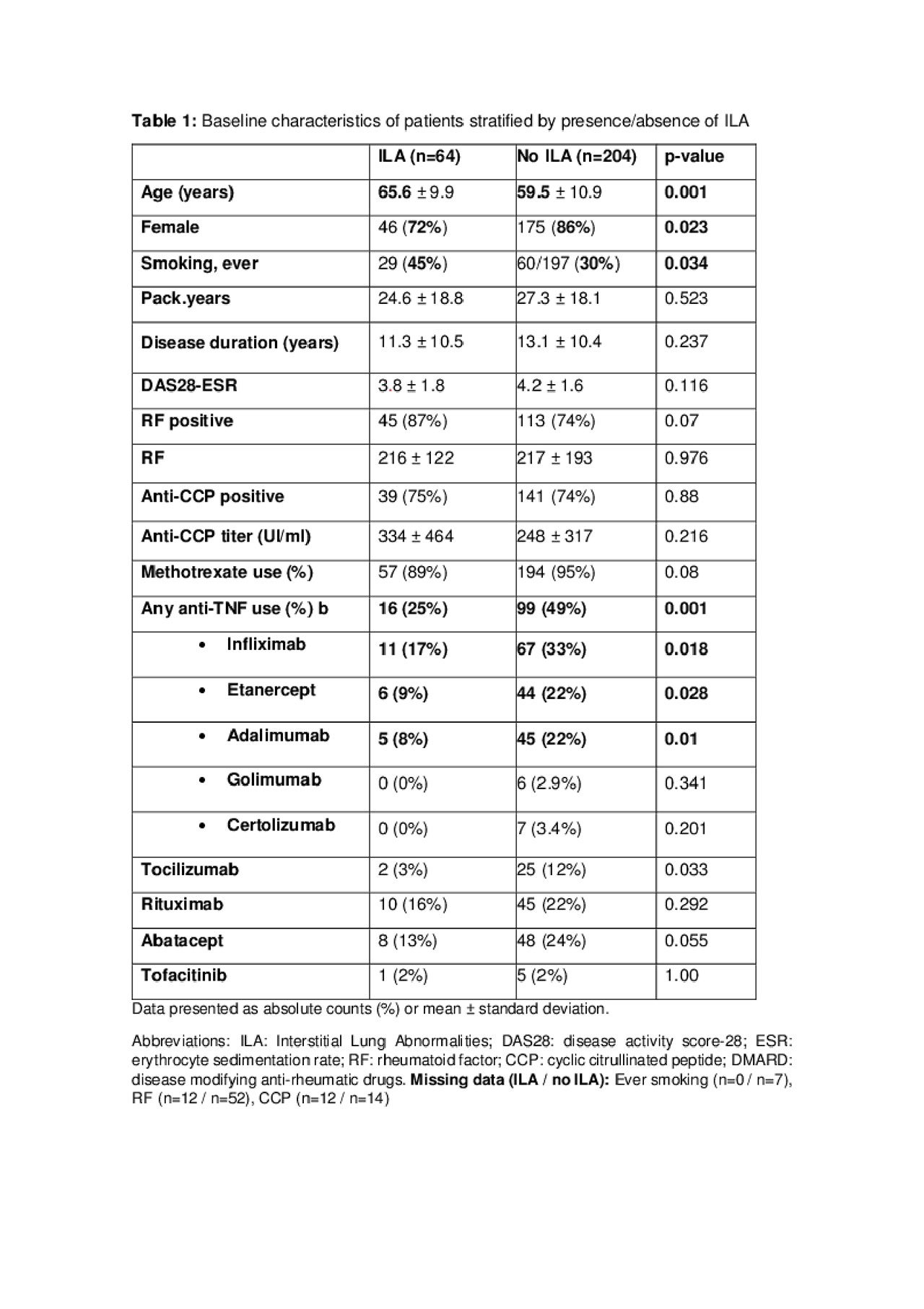
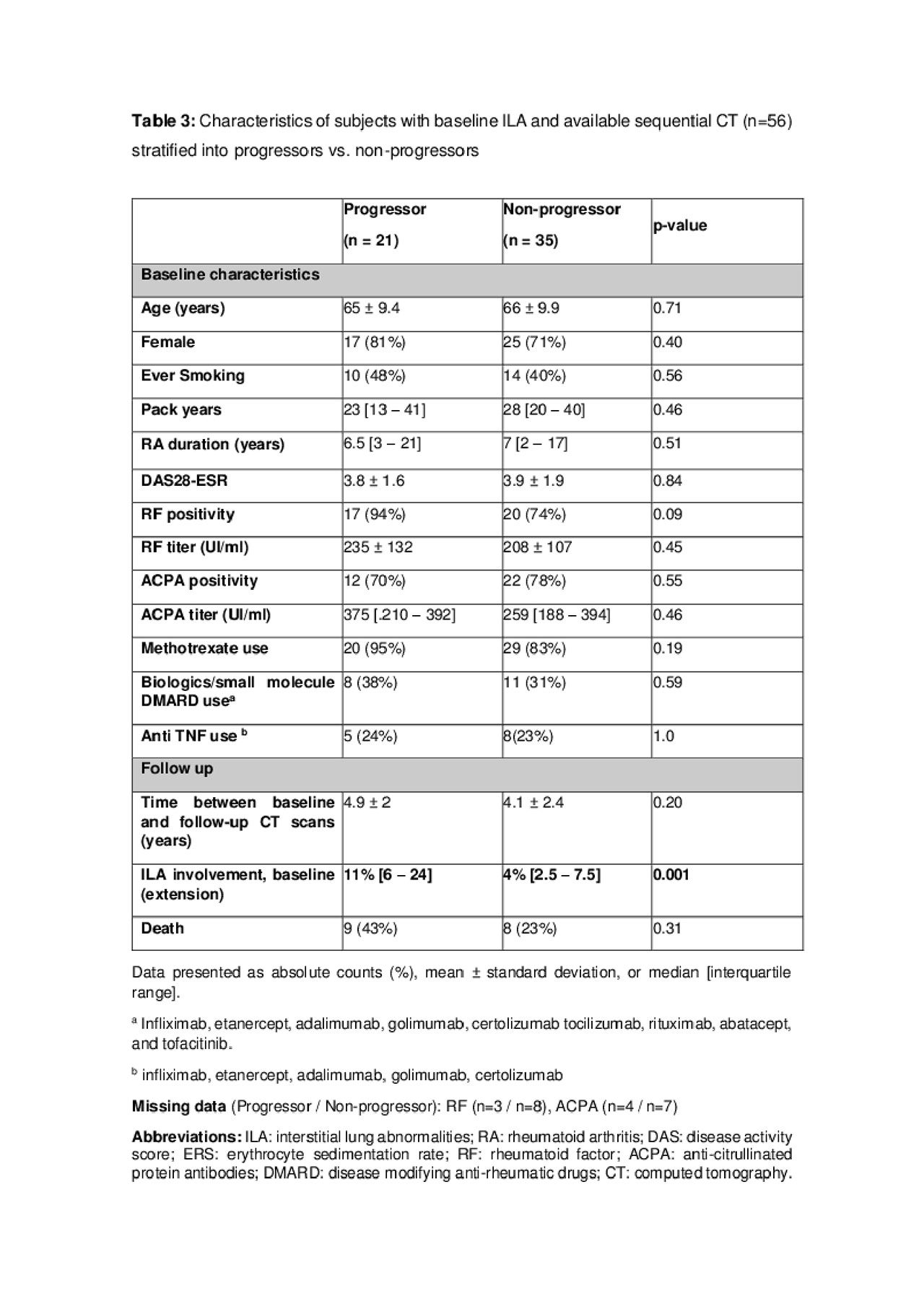
Results: 293 patients were scored for the presence of ILA. Chest CT were mostly indicated due to respiratory signs and/or symptoms (n = 131), but also not related to pulmonary indications (n = 115), and reasons not identified (n = 44). Twenty -five patients (9%) that presented indeterminate ILA were excluded from the analysis, remaining 268 patients. Sixty-four (22%) presented ILA, predominantly older male smokers, and less likely on biologics/small molecule disease-modifying anti-rheumatic drugs (table 1). The most common pattern of distribution observed was subpleural (table 2). Among ILA, 15 (43%) had usual interstitial pneumonia (UIP) or probable UIP on CT, 5 (14%) had nonspecific interstitial pneumonia (NSIP), and 15 (43%) had an unclassifiable pattern. Of the 56 ILA patients with sequential CTs, 38% had evidence of radiologic progression over 4.4 years.
Comparing “progressors group” with “non-progressors group”, the only statistically significant difference among the two groups was a higher median baseline ILA involvement in “progressors”. (table 3)
Conclusion: We identified that ILA in RA patients is characterized predominantly by UIP in a subpleural pattern, with an impressive high rate of progression in approximately four years. A lower frequency of biological/small molecules drugs in the non-ILA group is probably explained by a bias of indication due to pulmonary comorbidities. Greater baseline ILA extent, but not RA treatment (even methotrexate and anti TNF), was the most important risk factor for progression. Active surveillance is therefore recommended for these patients.
To cite this abstract in AMA style:
Bonfiglioli K, Sawamura M, Nakagawa R, Arimura F, Rangel D, Bueno C, Ribeiro A, Carvalho C, Bonfa E, Kairalla R, Kawano-Dourado L. Interstitial Lung Abnormalities in Rheumatoid Arthritis Patients: Identifying Associated Risk Factors [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/interstitial-lung-abnormalities-in-rheumatoid-arthritis-patients-identifying-associated-risk-factors/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/interstitial-lung-abnormalities-in-rheumatoid-arthritis-patients-identifying-associated-risk-factors/