Session Information
Date: Tuesday, November 12, 2019
Title: RA – Diagnosis, Manifestations, & Outcomes Poster III: Comorbidities
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Rheumatoid arthritis (RA) is a chronic inflammatory joint disease but also affects the cardiovascular (CV) system. Many patients are treated with corticosteroids. Corticosteroid use is associated with increased risk for cardiovascular events (CVE). We hypothesized that patients with RA who initiate corticosteroid therapy would have an increased risk for CVE related to dose and duration of corticosteroid use.
Methods: We investigated all RA patients enrolled in the Corrona registry between 10/2001-3/2018 who were not using prednisone at the time of enrollment and with at least one follow-up entry. Incident CVE were defined as physician-reported CVE captured in Corrona registry protocol (see Table 1). The enrollment visit date was the index date for estimating time to CVE. Survival analysis using Cox proportional hazard regression models were used to estimate adjusted hazard ratios (HR). Baseline covariables in the model adjusted for gender, age, race, duration of RA, history of CV disease, history of prednisone use, diabetes, hyperlipidemia, and/or hypertension, statin use, tobacco use, year of enrollment, the modified health assessment questionnaire score, and the clinical disease activity index (CDAI) for RA. Prednisone use and CDAI were included as time varying covariates. Several measures of prednisone use were considered: current dose; cumulative dose, and duration over the prior year and over the prior 6 months; weighted dose over 1 year and 6 months, with higher weights for more recent use. Data ranges for total dose and duration analyses were based on quartiles of prednisone use.
Results: 24,752 patients were eligible. 80,501 patient years of follow-up were analyzed. The overall rate of CVE was 1.75/100 person years (95% CI 1.66-1.84/100 person years). Table 1 shows HR and 95% confidence intervals (CI) for the various models. Current prednisone dose showed an increased risk at 5-9mg (HR=1.47) and ≥10mg (HR=1.56). Cumulative prednisone dose at 6 months showed increased risk at 811-1100mg (HR=1.42) and >1100mg (HR=1.55); weighted dose showed increased risk at 811-1100mg (HR=1.49) and >1100mg (HR=1.52). Cumulative prednisone duration at 6 months showed increased risk at >181 days (HR=1.48). Cumulative prednisone dose at 1 year showed increased risk at 1101-2100mg (HR=1.30) and >2100mg (HR=1.54); weighted dose shows increased risk for >2100mg (HR=1.69). Cumulative prednisone duration at 1 year showed increased risk for >360 days (HR=1.70).
Conclusion: For patients with RA who initiate corticosteroid use, there is an increased CVE risk associated with daily dose, cumulative dose over the last six months and one year, and duration of use. Physicians should counsel patients on the increased CVE risk and consider interventions to minimize risk.
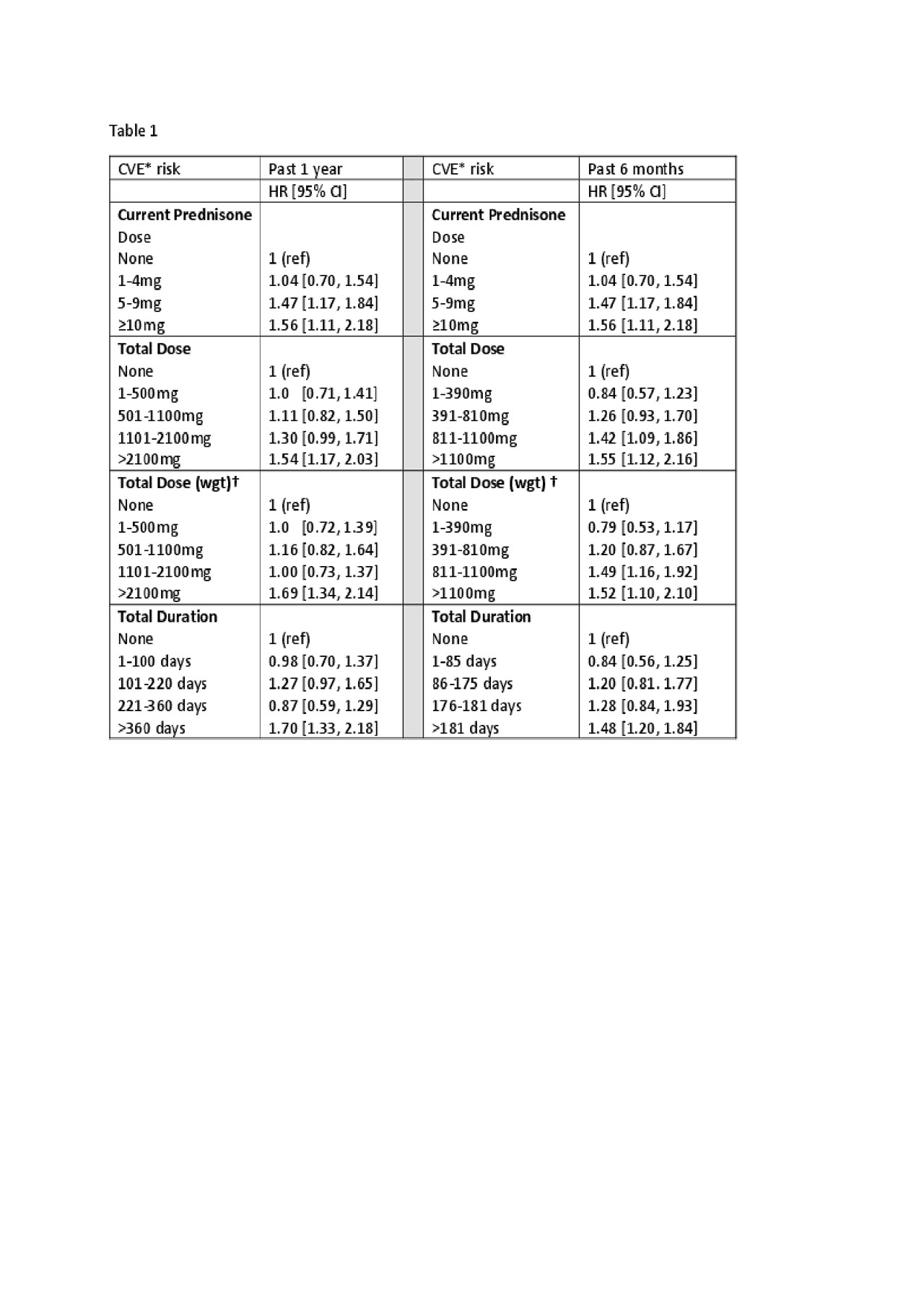
RA and Steroids_ACR_Abstract_Table
To cite this abstract in AMA style:
Ocon A, Reed G, Kremer J. In Rheumatoid Arthritis, New-onset Prednisone Use Is Associated with a Daily Dose, Cumulative Dose, and Duration-dependent Risk for Cardiovascular Events at 6 Months and 1 Year of Use [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/in-rheumatoid-arthritis-new-onset-prednisone-use-is-associated-with-a-daily-dose-cumulative-dose-and-duration-dependent-risk-for-cardiovascular-events-at-6-months-and-1-year-of-use/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/in-rheumatoid-arthritis-new-onset-prednisone-use-is-associated-with-a-daily-dose-cumulative-dose-and-duration-dependent-risk-for-cardiovascular-events-at-6-months-and-1-year-of-use/
