Session Information
Date: Tuesday, November 12, 2019
Title: RA – Diagnosis, Manifestations, & Outcomes Poster III: Comorbidities
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Inflammation accounts for much of the excess cardiovascular disease (CVD) in patients with rheumatoid arthritis (RA). We hypothesize that increased systemic inflammation leads to vascular endothelial dysfunction and coronary microvascular dysfunction (CMD). CMD in the general population is associated with increased risk for cardiac mortality, however, there are limited data on CMD in RA. The objective of this study was to study the associations between RA clinical factors with CMD.
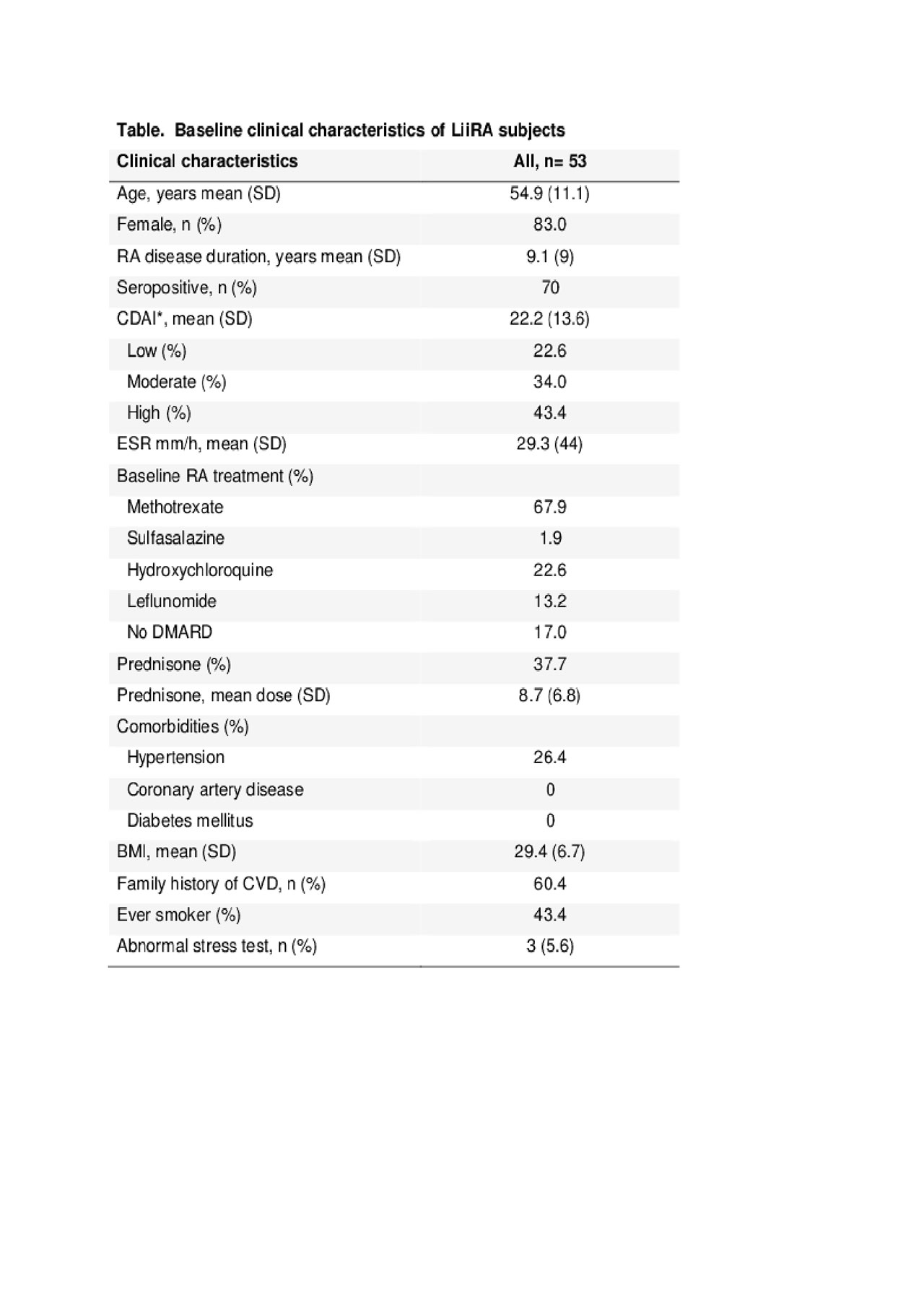
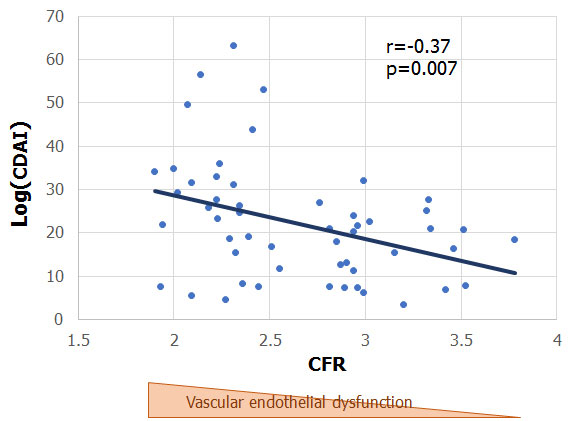
Methods: We used interim baseline data from the first 53 subjects enrolled in the Lipids, Inflammation, and CV Risk (LiiRA, ClinicalTrials.gov: NCT02714881) study. Briefly, the LiiRA study enrolls RA patients, age >35, about to initiate tumor necrosis factor inhibitor (TNFi) therapy. Exclusion criteria include statin use, prednisone dose or equivalent >10mg, or biologic DMARD use in the past 6 months. Demographics, RA clinical factors, and clinical disease activity index (CDAI) were collected. All subjects underwent a stress myocardial perfusion PET scan (cardiac PET), a routine clinical stress test at our institution. The cardiac PET quantifies myocardial blood flow (MBF) at rest and during maximal hyperemia in response to a stress agent, regadenoson. Coronary flow reserve (CFR) is a ratio of MBF during maximal hyperemia over that at rest. A lower CFR in the absence of obstructive coronary artery disease (CAD) is indicative of CMD. We tested correlations between RA clinical factors with CFR. Our primary analysis tested the association between CDAI and CFR adjusted by age, gender, and smoking status.
Results: The mean age of subjects in LiiRA was 55 years, 83% were female, 70% seropositive, with a mean RA disease duration of 9.1 years (Table). No patients had history of CAD or DM, and 26% had a history of hypertension. Three patients (5.3%) had mildly abnormal perfusion scans at baseline. Higher CDAI was correlated with a lower CFR, r=-0.37, p=0.007 (Figure); this association remained significant after adjusting for age, gender, and smoking status (p=0.004). Other clinical factors associated with a significantly lower CFR were older age, r=-2.8, p=0.04, and a higher tender joint count, r=-0.34, p=0.01. We observed no correlation between DMARD or prednisone use at baseline with CFR.
Conclusion: Among RA patients with no history of overt CAD and low prevalence of CV risk factors, higher RA disease activity was associated with a higher degree of CMD. These findings support a mechanistic pathway whereby inflammation may lead to increased CV risk through microvascular dysfunction. Studies are underway to determine whether CMD is modifiable with RA treatments.
To cite this abstract in AMA style:
Huang S, He Z, Solomon D, Massarotti E, Golnik C, Seyok T, Brownmiller S, Cai T, Yang N, Campbell L, Barrett L, Bibbo C, Pariser K, Todd D, Bolster M, Di Carli M, Liao K. The Association Between Disease Activity with Coronary Microvascular Dysfunction in Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/the-association-between-disease-activity-with-coronary-microvascular-dysfunction-in-rheumatoid-arthritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-association-between-disease-activity-with-coronary-microvascular-dysfunction-in-rheumatoid-arthritis/