Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with chronic illness often face challenges with their sexual health and intimacy. The issues can be inherent to the disease state, self-image, or physiologic function. Sexual health, function and intimacy issues are rarely included in the health assessment questionnaires and disability indices used by Rheumatologists. In addition, Rheumatologists may be ill equipped to ask and respond to patients’ inquiries about sexual function. Most providers acknowledge the impact of a patient’s disease on their sexual health, but admitted this area is often neglected. The purpose of this study was to learn about rheumatology care providers’ practices when speaking to patients about sexual health and intimacy. Despite the extensive data suggesting the widespread, negative impact of chronic illness on sexual health, we hypothesize that there is a lack of training for providers about how to address sexual health and intimacy issues. We intend to use this information to develop a provider education program so they may provide better care for patients.
Methods: Rheumatology Health Care Providers (HCPs), including Rheumatologists, Nurse Practitioners, and RNs, were asked to complete a 31 item questionnaire (N=50). The survey was designed to understand current practices and potential reasons why providers fail to address sexual health with patients. Ten questions addressed provider awareness of the effects of rheumatologic disease on sexual health, discussion of these topics, and if patients were referred to other providers for assistance. Survey questions also assessed the effect of lack of time, and lack of training or experience in addressing sexual health issues. Each response was that of a five point Likert scale.
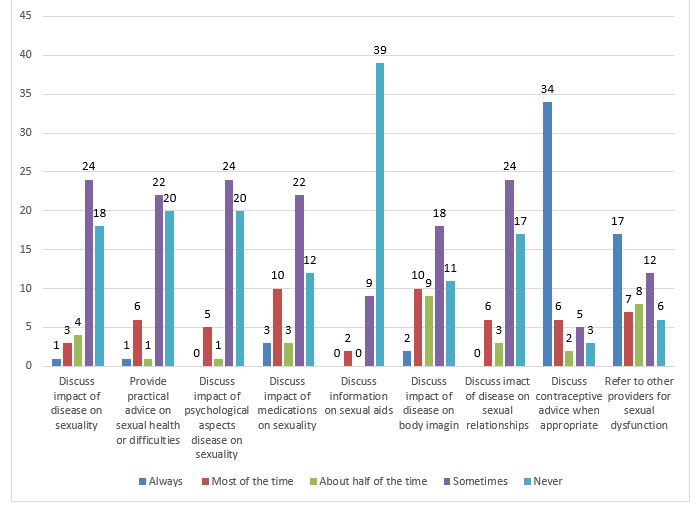
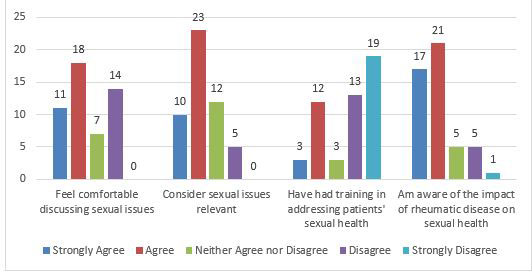
Results: Of the 50 HCPs who completed the survey, 48% reported that they discuss the impact of a patient’s disease on their sexuality, and the impact of psychological aspects of disease on sexuality “sometimes.” However, 36% and 40% of responders report that they “never” discuss either of the two topics, respectively. Additionally, 48% “sometimes” and 34% “never” discuss the impact of disease on patients’ sexual relationships. Notably, 78% of HCPs never provide information about sexual aids. The majority of responders reported lack of skills/knowledge about sexual health, patient embarrassment, and patient age as barriers, while lack of time and privacy were noted to significantly interfere with providers’ discussion of sexual health. Finally, 66% of HCPs agree or strongly agree that sexual health issues are relevant to rheumatology practice.
Conclusion: The impact of rheumatologic disease on sexual health cannot be underestimated. The results of this study highlight the barriers to discussing sexual health with patients, most significantly, a lack of knowledge about the topic. Additionally, more than half of survey responders agree that sexual health issues should be addressed, indicating an interest in the topic. We intend to use this information to develop a training program for rheumatology HCPs with the goal of educating providers about how to address and guide patients about their sexual health and intimacy issues.
To cite this abstract in AMA style:
Schwartzman-Morris J, Leo A, Nandkumar P. Sexual Health, Intimacy and Rheumatology Practices [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/sexual-health-intimacy-and-rheumatology-practices/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/sexual-health-intimacy-and-rheumatology-practices/