Session Information
Date: Tuesday, November 12, 2019
Title: Patient Outcomes, Preferences, & Attitudes Poster II: Patient Preferences, Beliefs, & Experiences
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Physical Activity (PA) is beneficial for people with inflammatory arthritis (IA). In 2018, EULAR published the first recommendations for guiding PA in patients with IA.1These endorsed the American College of Sports Medicine-American Heart Association Public Health Recommendations, which encourage participation in four domains of PA: Aerobic, Resistance, Flexibility, and Balance. They also included provider recommendations for PA promotion and delivery to patients with IA. Objectives of our study were to 1) Describe levels of participation in the four PA domains in an IA population; 2) Identify barriers/facilitators to PA; 3) Explore patient views on importance of PA; and 4) Investigate if EULAR recommendations for promotion/delivery of PA are being incorporated into care.
Methods: Patients with IA from a university rheumatology practice were invited in person or via the medical record to take an 81-question, 15-minute survey. The survey asked in which PA domains they participated, about facilitators/barriers to PA, and whether the recommendations for PA promotion had been addressed during their care. Respondents reporting minimum aerobic exercise for 20 minutes three times weekly plus at least one other domain were categorized into an “Active” group, others were categorized as “Inactive.” Patient characteristics and survey responses were compared between groups using t-test for continuous and Chi-squared or Fisher’s-Exact Test for categorical variables.
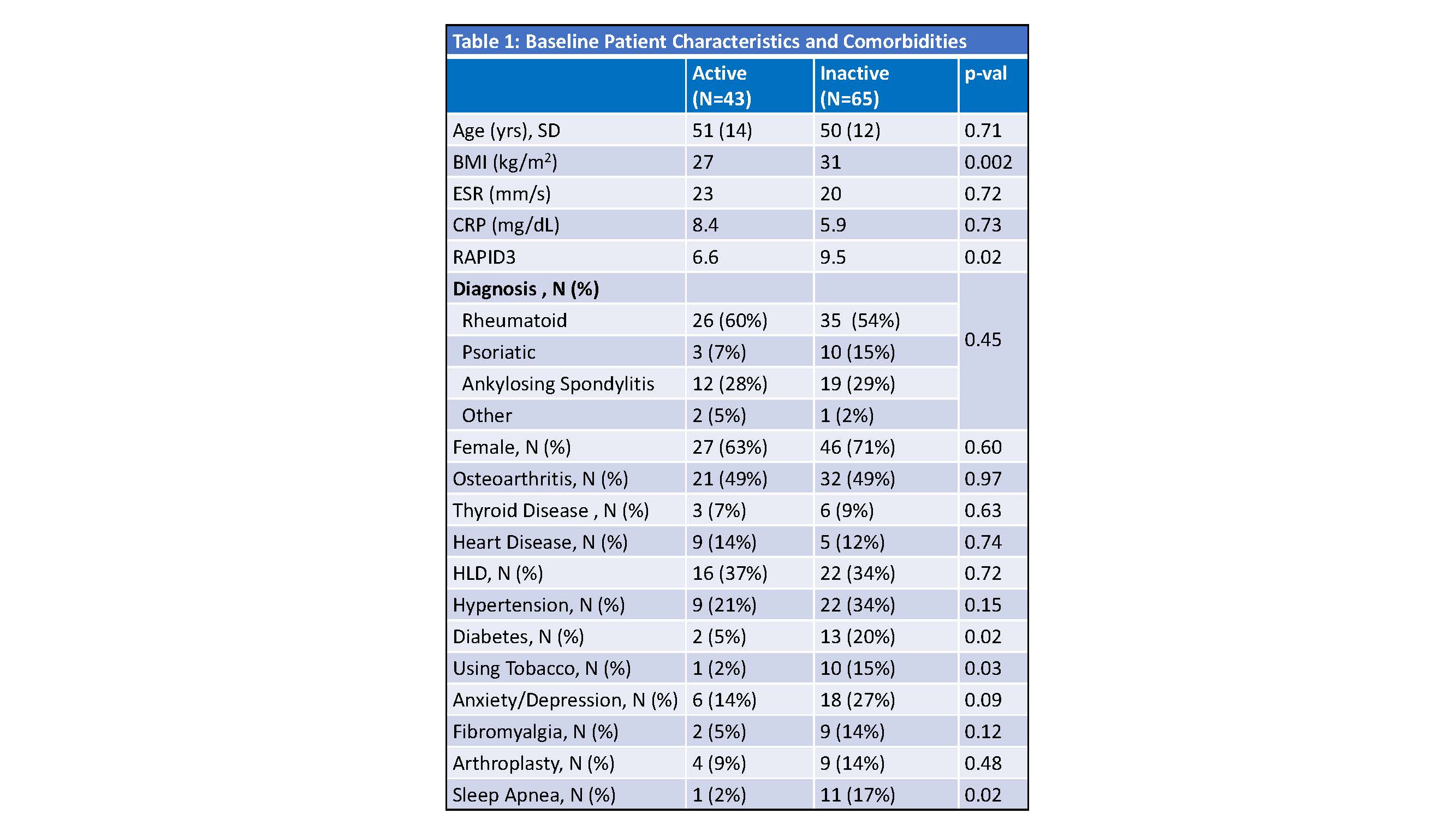
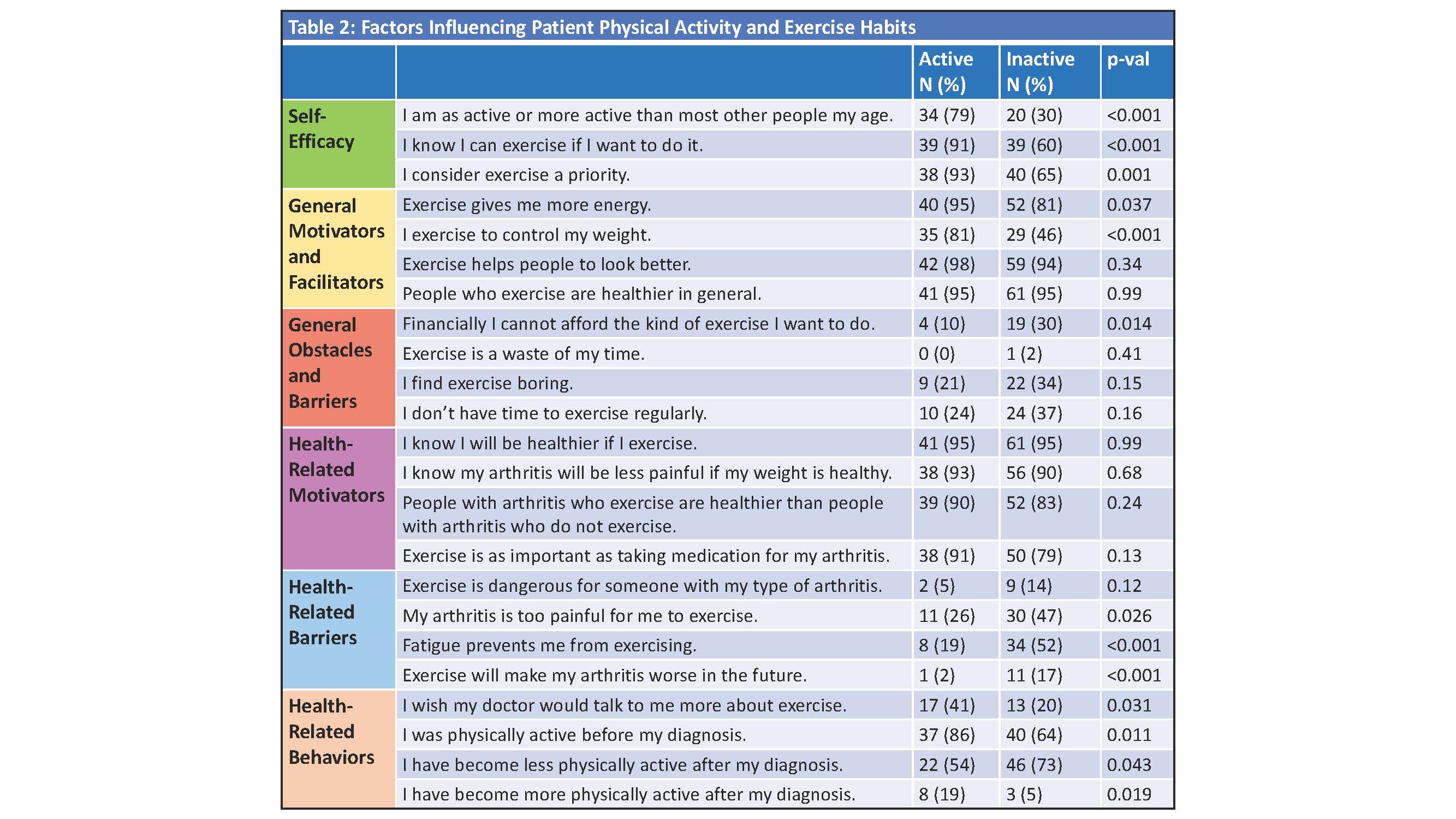
Results: Of 1,113 patients invited, 108 participated. Sixty (43%) reported aerobic exercise, 44 (41%) flexibility, 42 (39%) resistance, and 18 (17%) balance. Forty-three (40%) were categorized as active and 65 (60%) as inactive. The active group had lower BMI and lower RAPID3 Scores, and fewer people with diabetes, sleep apnea, and tobacco use (Table 1). A larger proportion of the active group reported self-efficacy for exercise (p< 0.001), prioritizing exercise (p=0.01), exercising for weight control (p< 0.001) and improved energy with exercise (p=0.04). A larger proportion of the active group (86%) also reported PA engagement prior to arthritis diagnosis (p=0.01). More patients in the inactive group compared to the active group cited finances (p=0.01), pain (p=0.03), fatigue (p< 0.001), and concern that PA worsens arthritis (p >0.001) as barriers . Most patients (in both groups) understood the health-related benefits of PA (Table 2). A minority of patients in both groups perceived recommendations about PA were addressed in clinical care (Table 3).
Conclusion: While about half of patients with IA reported aerobic exercise, most do not engage in resistance, flexibility, or balance training despite recommendations. Overall, patients acknowledge the benefits of PA, but do not perceive that they receive advice regarding PA from doctors and most habits are formed without instruction from rheumatologists. With new EULAR guidelines, there is an opportunity for providers to have more prescriptive discussions about exercise.
1: Rausch Osthoff, et al. 2018 EULAR recommendations for PA in people with Inflammatory Arthritis and Osteoarthritis. Ann Rheum Dis. 2018:1251–60.
To cite this abstract in AMA style:
Freid L, Ogdie A, Baker J. Prescribing Exercise: Facilitators and Barriers to the Successful Implementation of Physical Activity Guidelines in Inflammatory Arthritis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/prescribing-exercise-facilitators-and-barriers-to-the-successful-implementation-of-physical-activity-guidelines-in-inflammatory-arthritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/prescribing-exercise-facilitators-and-barriers-to-the-successful-implementation-of-physical-activity-guidelines-in-inflammatory-arthritis/