Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Among rheumatoid arthritis (RA) patients, pain may be due to peripheral inflammation or other causes, such as central pain mechanisms. The objective was to use self-report measures and physical examination to identify clusters of RA patients who may have diverse causes of pain and different prognoses and treatment options.
Methods: Data were analyzed from 169 RA patients in a prospective observational study who had any pain > 0/10 and completed questionnaires about pain, fatigue, depression, anxiety, catastrophizing and sleep problems. Systemic inflammation was assessed using serum C-reactive protein (CRP) levels. A hierarchical agglomerative clustering procedure with Ward’s method was used to obtain subgroups. Multivariate analysis of variance was used to determine the contribution of each variable in a cluster. General linear regression models were used to examine differences in clinical characteristics across subgroups. Discriminant analyses were performed to determine coefficients for linear combinations of variables that assigned cluster membership to individual cases.
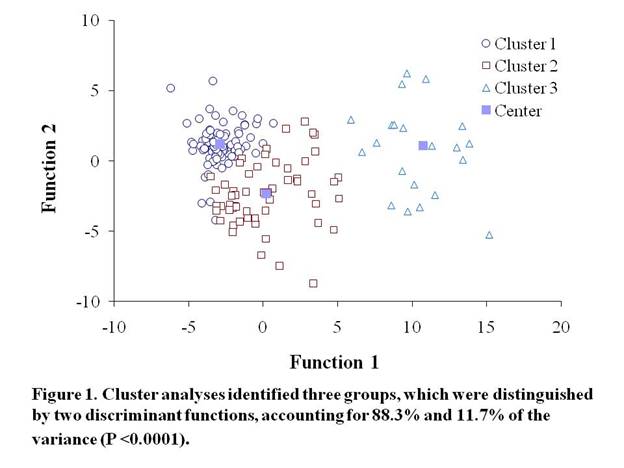
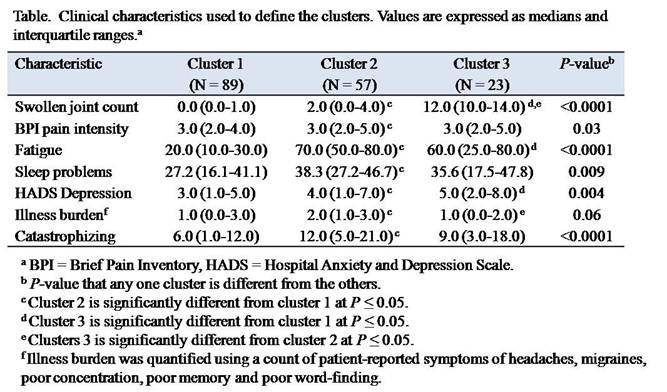
Results: Cluster analyses identified three groups of RA patients (Figure). Cluster 1 consisted of the largest number of patients (N = 89, 52.7%) and was characterized by the lowest swollen joint counts and the lowest levels of fatigue and depression (Table). Cluster 2 consisted of 57 participants (33.7%), characterized by low swollen joint counts and high levels of fatigue, catastrophizing and sleep problems, indicative of a chronic widespread pain syndrome. Cluster 3 consisted of 23 participants (13.6%), characterized by high swollen joint counts and moderate levels of fatigue, catastrophizing and sleep problems, consistent with active inflammatory disease.
Conclusion: Although most patients had low levels of inflammation, pain and fatigue, 47.3% continued to report moderate to high pain and fatigue. These results indicate that: 1) chronic widespread pain syndromes are common among patients with established RA; 2) active inflammatory disease does not explain all problems with pain, fatigue and psychosocial problems; and 3) chronic widespread pain syndromes are associated with significantly diminished quality of life (assessed by depression, fatigue and sleep problems), even compared to patients with active inflammatory disease.
Disclosure:
Y. C. Lee,
Forest Research Insitutute,
2,
Merck Pharmaceuticals,
1,
Novartis Pharmaceutical Corporation,
1,
Cubist,
1,
Elan Corporation,
1;
M. A. Frits,
None;
C. K. Iannaccone,
None;
M. E. Weinblatt,
MedImmune,
2,
Crescendo Biosciences,
2,
Bristol-Myers Squibb,
2,
MedImmune,
5,
Crescendo Biosciences,
5,
Bristol-Myers Squibb,
5;
N. A. Shadick,
MedImmune,
2,
Crescendo Biosciences,
2,
Amgen ,
2,
Abbott Immunology Pharmaceuticals,
2,
Genentech and Biogen IDEC Inc.,
2;
D. A. Williams,
Pfizer Inc,
5,
Forest Laboratories,
5,
Eli Lilly and Company,
5,
Healthy Focus, Inc.,
5;
J. Cui,
None.
« Back to 2013 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/subgrouping-of-rheumatoid-arthritis-patients-based-on-pain-fatigue-inflammation-and-psychosocial-factors/