Session Information
Date: Monday, November 11, 2019
Title: 4M097: Systemic Sclerosis & Related Disorder – Clinical II: Cardiopulmonary Involvement (1830–1835)
Session Type: ACR Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: Pulmonary disease is a leading cause of mortality in scleroderma (SSc). Previous studies indicate that the coexistence of pulmonary hypertension (PH) and interstitial lung disease (ILD) is associated with worse survival. However, this has not been uniformly confirmed, in part due to lack of refined categorization of ILD extent and PH assessment by invasive testing. In addition, the clinical burden of disease has not been fully explored in different SSc lung disease subtypes. Therefore, we sought to define outcomes related to type and severity of lung involvement in a well characterized SSc cohort enriched for pulmonary disease.
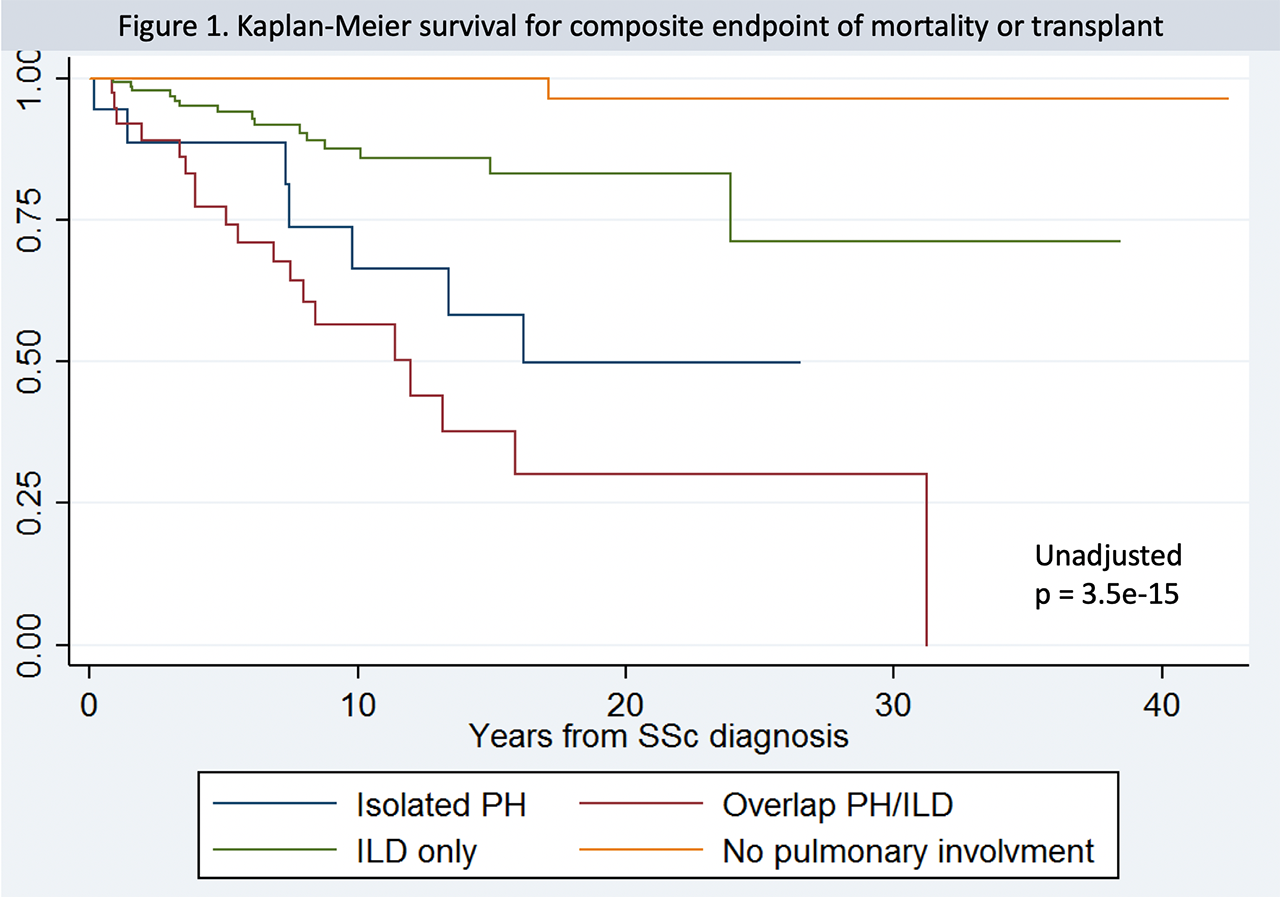
Methods: A retrospective analysis was conducted on 355 SSc subjects stratified into the following subgroups: isolated ILD, isolated pulmonary arterial hypertension (PAH, WHO Group I), overlap ILD/PH (WHO Group I and/or Group III), or SSc without pulmonary disease. PH was confirmed by right heart catheterization according to standard definition. PH due to left heart disease (Group II) was excluded. ILD was confirmed by chest CT. Biannual assessments of clinical and functional data and patient reported outcomes (PROs) were included. Hospitalization for heart or respiratory failure and mortality were ascertained by medical record review. Continuous variables were compared by Student’s t-test or Wilcoxon’s rank sum test. Categorical variables were compared using chi-square. A composite outcome of mortality or lung transplant was assessed by Kaplan-Meier analysis and adjusted Cox proportional hazard models.
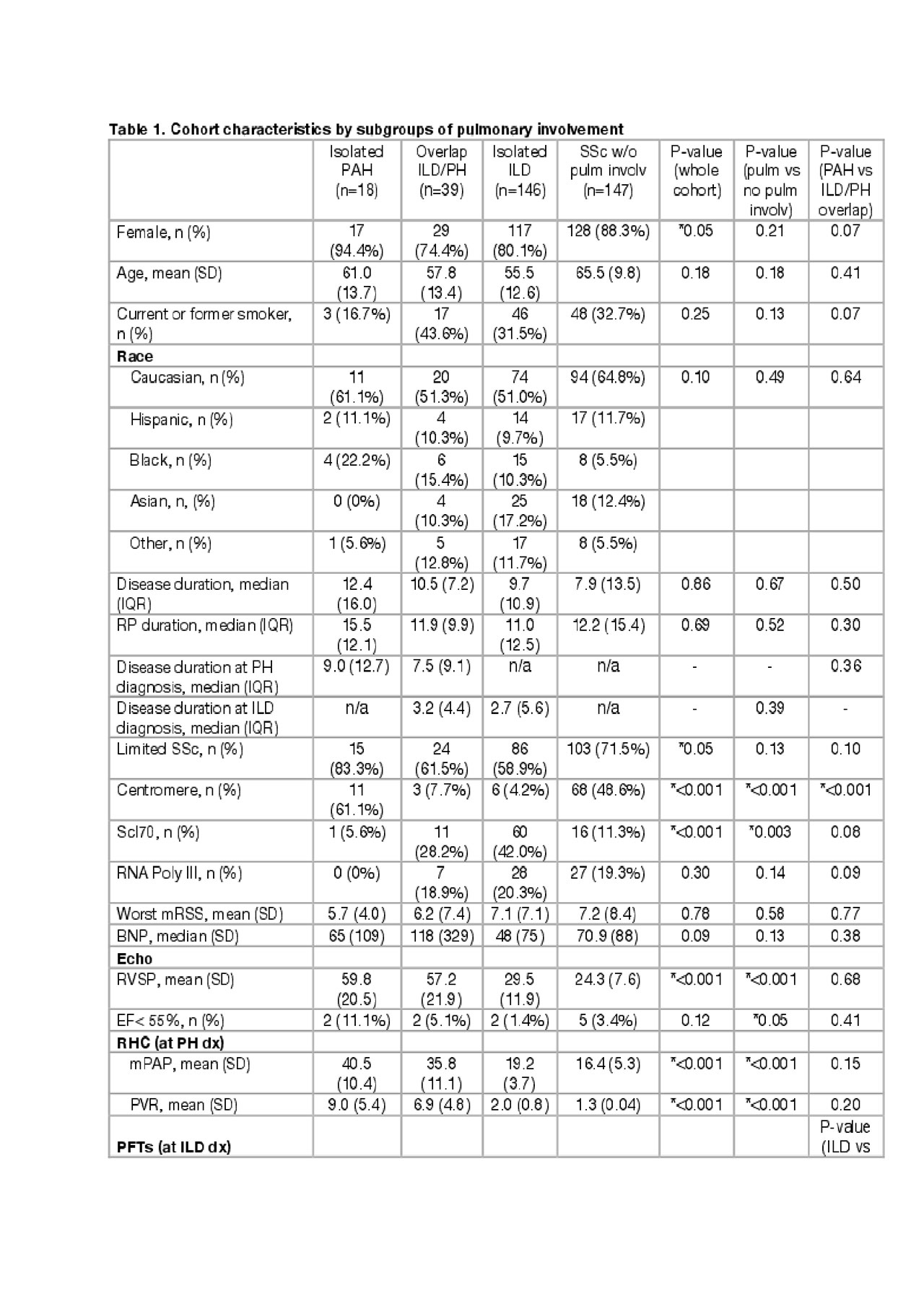
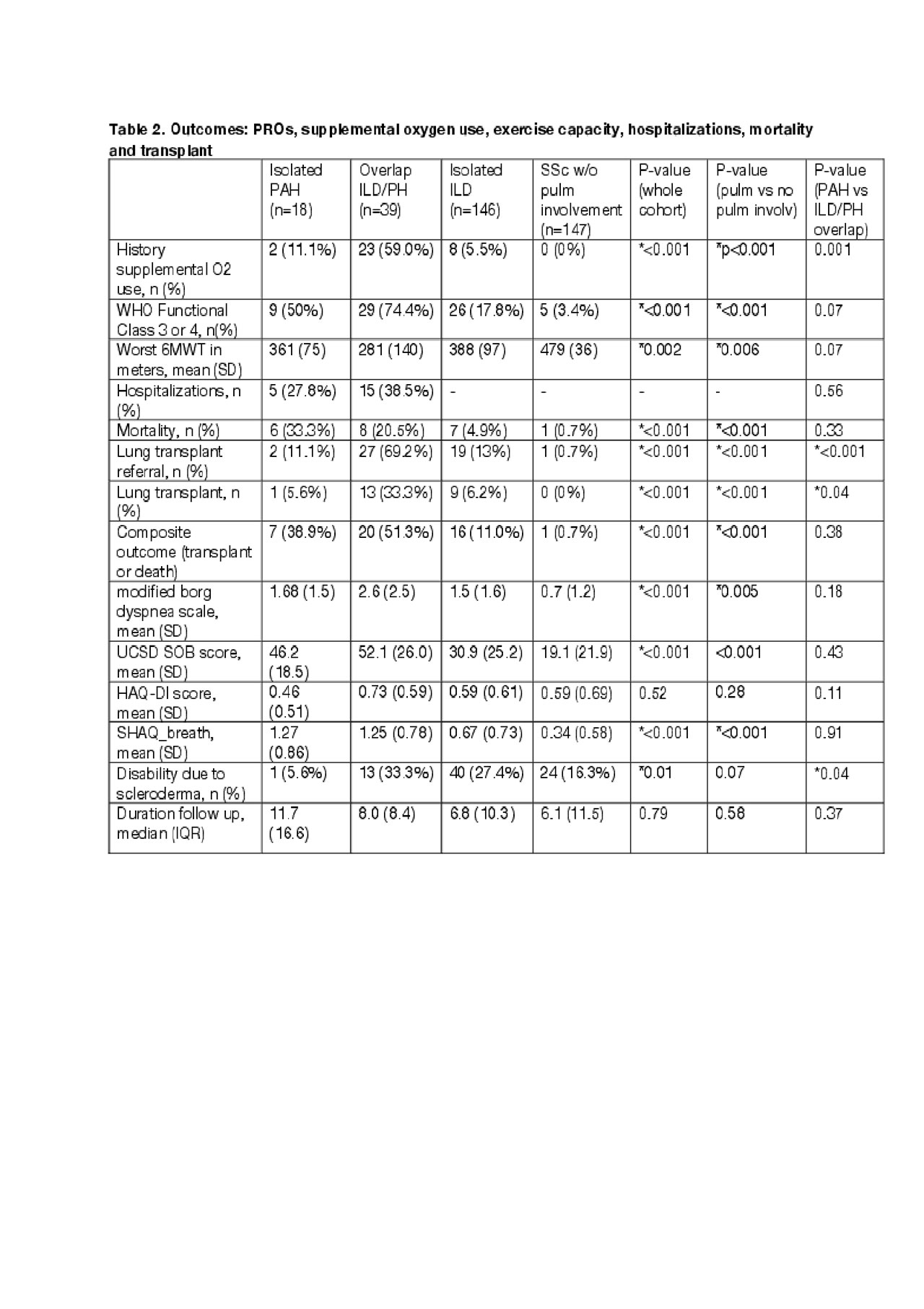
Results: Differences among pulmonary subtypes characteristics are shown in Table 1. A significantly higher proportions of males in ILD/PH, of limited SSc and centromere positivity in PAH, of SCL70 in ILD and ILD/PH were noted. Baseline hemodynamics and PH therapy did not differ significantly between PAH and overlap ILD/PH. Subjects with PH/ILD showed more severe restrictive lung disease at ILD diagnosis compared to ILD only (FVC 1.99±0.71 vs 2.48±0.72, p=0.002) with ILD preceding PH onset more commonly (89.7%). Among pulmonary SSc sybtypes, overlap ILD/PH was significantly associated with worse functional capacity (WHO Functional Class and 6-minute walk distance), greater requirement for supplemental oxygen, greater SSc-related disability, and higher mean dyspnea PRO scores (Table 2). Notably, ILD/PH subjects compared to PAH and ILD also showed significantly increased rates of referral for lung transplant (69% vs 11% vs 13; p=< 0.001) as well as of transplant itself (33.3% vs. 5.6% vs 6.2%; p=< 0.001). This may explain the lack of difference in mortality between PAH and ILD/PH in this cohort. In fact, death or transplant free survival was significantly worse in the PH/ILD group (Figure 1; p = 3.5e-15).
Conclusion: The disease burden of lung involvement in SSc is significant, particularly in subjects with concurrent PH (Group I and III) and ILD. This subset manifests more advanced respiratory symptoms and functional decline compared to PAH and ILD alone. Referral for lung transplantation is confirmed as a life-saving intervention for patients with SSc lung involvement.
To cite this abstract in AMA style:
French S, Taylor K, Rush S, Boin F. Subtypes of Scleroderma Lung Involvement Associated with Burden of Disease and Outcomes [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/subtypes-of-scleroderma-lung-involvement-associated-with-burden-of-disease-and-outcomes/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/subtypes-of-scleroderma-lung-involvement-associated-with-burden-of-disease-and-outcomes/