Session Information
Date: Monday, November 11, 2019
Title: Pediatric Rheumatology – ePoster II: SLE, Juvenile Dermatomyositis, & Scleroderma
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Antiphospholipid antibodies (aPL) have been extensively reported in children; however, research on thrombotic risks associated with aPL among pediatric patients is scarce. Positive aPL are not uncommon in pediatric connective tissue diseases, but identification and management of these patients is challenging due to lack of validated criteria and a paucity of data. Misconceptions surrounding clinically significant aPL profiles may lead to missed diagnoses or incorrect diagnoses of APS, and many asymptomatic patients are managed with prophylactic ASA without a clear understanding of risk factors for thrombosis. Our aim is to identify additional risk factors for thrombosis in a unique cohort of pediatric aPL positive carriers.
Methods: Retrospective chart review was performed on 491 pediatric patients with connective tissue diseases seen in our institution from 2001 to 2019. Patients without persistently moderate to high titer aPL at least 12 weeks apart were excluded. Univariate analysis was performed to evaluate the relationship between different risk factors and arterial/venous thrombosis.
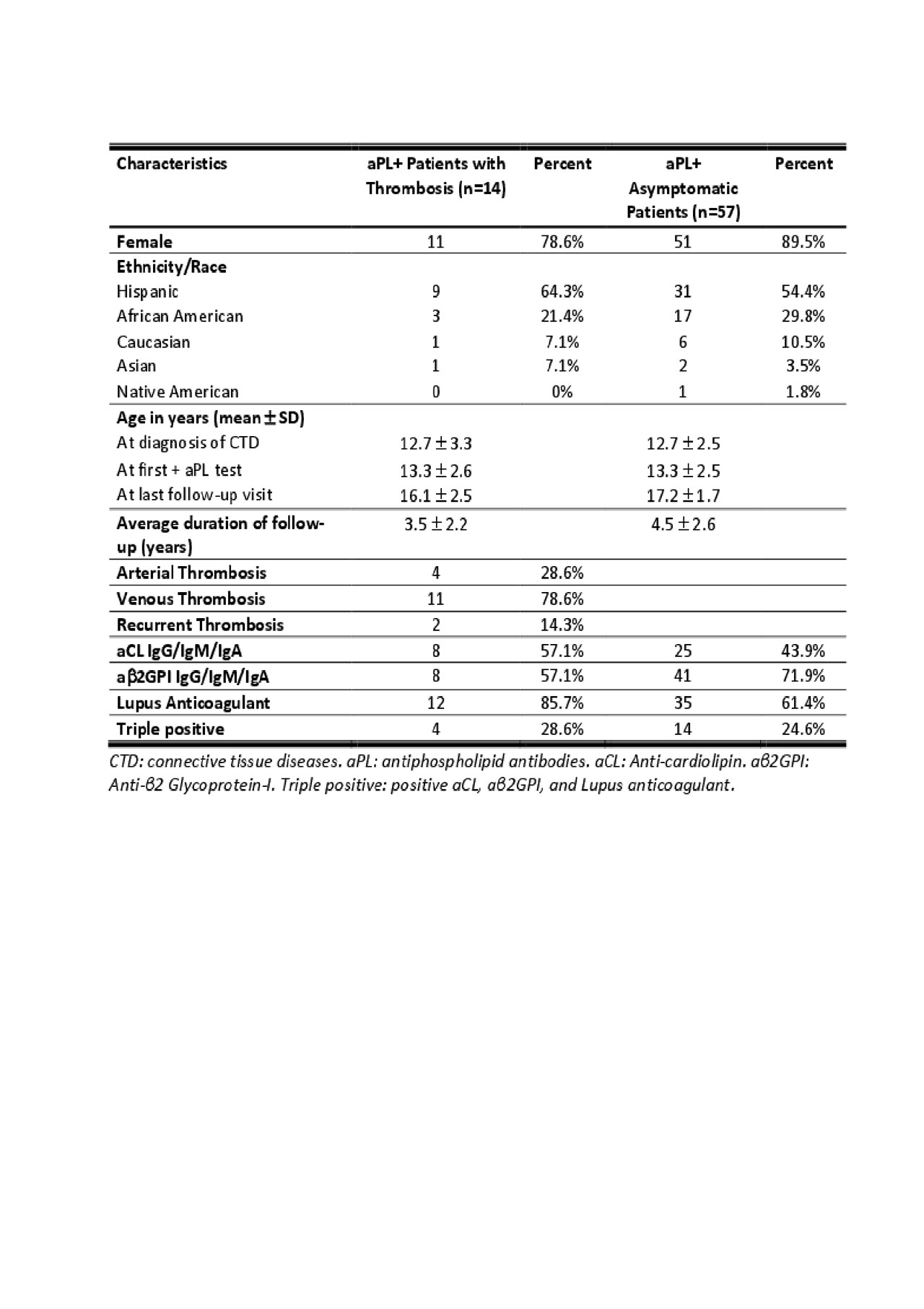
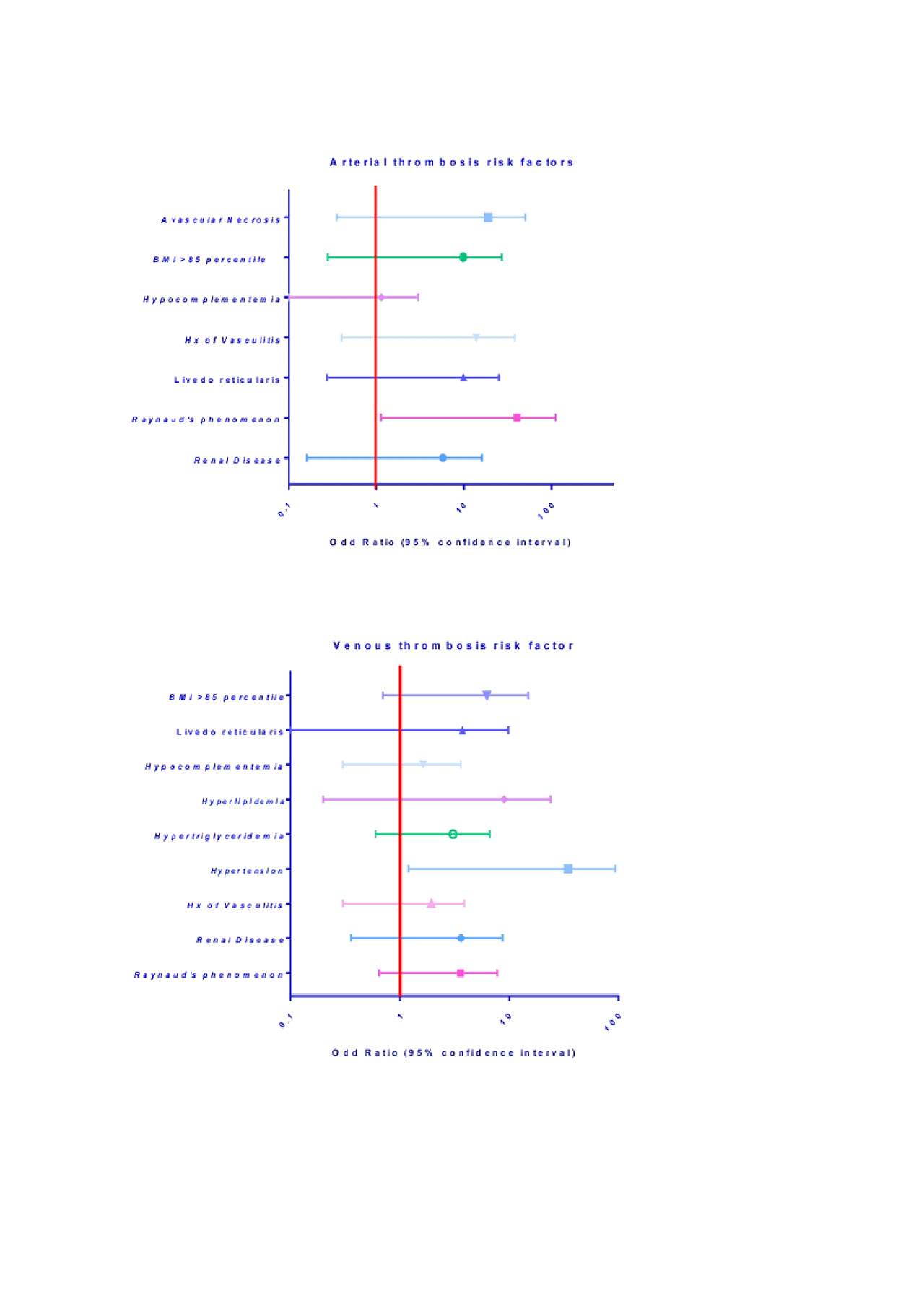
Results: Seventy-one aPL positive children with underlying connective tissue diseases are included in this cohort (Table 1). The majority (87%) are female and of Hispanic ethnicity (56%). Mean age of the cohort at the diagnosis of connective tissue disease is 12.7 (SD 2.6) years, and mean age of first positive aPL is 13.3 (SD 2.5) years. Average length of follow-up is 4.3 (SD 2.5) years. Four (5.6%) patients had arterial thrombosis, and 11 (15.5%) had venous thrombosis. Fifty-seven (80.3%) patients did not have any thromboembolic events. Among traditional risk factors and signs of endothelial injury, only Raynaud’s phenomena demonstrated significant association with arterial thrombosis (OR=8.4, 95%CI 1.13 – 111, P=0.039), and hypertension or antihypertensive use demonstrated significant association with venous thrombosis (OR=8.387, 95%CI 1.2 – 94, P=0.02) (Figure 1). Of the asymptomatic patients, forty-six (81%) were placed on long-term low dose ASA for primary thrombosis prophylaxis. Our investigation also identified several real-world clinical challenges, including variations in reference ranges for aPL studies over time and between reporting laboratories, inconsistencies in interpretation of aPL profiles by providers, over-identification of positive aPL, and subsequent over-utilization of prophylactic ASA without sufficient supporting evidence.
Conclusion: Data from our cohort suggests that Raynaud’s phenomenon is a potential predictor of arterial thrombosis and the presence of hypertension or anti-hypertensive medication use is a potential predictor of venous thrombosis in aPL positive pediatric carriers. Due to lack of validated criteria and standardized clinical guidelines specifically for pediatric patients, identification and subsequent management of aPL positivity in this population remains problematic for clinicians. Further studies investigating pediatric aPL profiles and risk factors for development of thrombosis are needed to help guide clinicians in caring for these challenging patients.
To cite this abstract in AMA style:
Sloan E, Wright T, Zuo Y. Identifying Additional Risk Factors for Arterial and Venous Thrombosis Among Pediatric Antiphospholipid Antibodies Carriers [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/identifying-additional-risk-factors-for-arterial-and-venous-thrombosis-among-pediatric-antiphospholipid-antibodies-carriers/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/identifying-additional-risk-factors-for-arterial-and-venous-thrombosis-among-pediatric-antiphospholipid-antibodies-carriers/