Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Blood pressure follows a circadian rhythm; usually systolic blood pressure (SBP) drops by more than 10% during the night. Absence of this phenomenon, known as “non-dipping” is a cardiovascular risk factor independent of hypertension. Patients with systemic lupus erythematosus (SLE) have a high prevalence of hypertension and cardiovascular event risks, but little is known about nocturnal blood pressure dipping in patients with SLE and its association with inflammatory markers.
Methods: Twenty-six patients with SLE and 26 control subjects frequency-matched for age, race and sex were included in this study. All subjects were 18 years of age or older. Patients with SLE met the American College of Rheumatology revised classification criteria for SLE. Control subjects did not have SLE or other autoimmune diseases. We calculated nocturnal blood pressure dipping using data from ambulatory 24-hour blood pressure measurements. Blood pressure measurements were divided into daytime and nighttime periods defined by the patients’ reported hours of sleep. The average systolic blood pressure (mm Hg) was obtained for each period, and the nighttime/daytime systolic blood pressure ratio was calculated. We measured plasma concentrations of 92 inflammation-related markers using a multiplex immunoassay (Inflammation panel; Olink Bioscience, Uppsala, Sweden). Wilcoxon-rank sum tests and Fisher exact test were used to compare blood pressure results between patients with SLE and control subjects. Spearman correlations were used to assess the correlation between blood pressure night dipping (expressed in %) and the inflammatory biomarkers in patients with SLE.
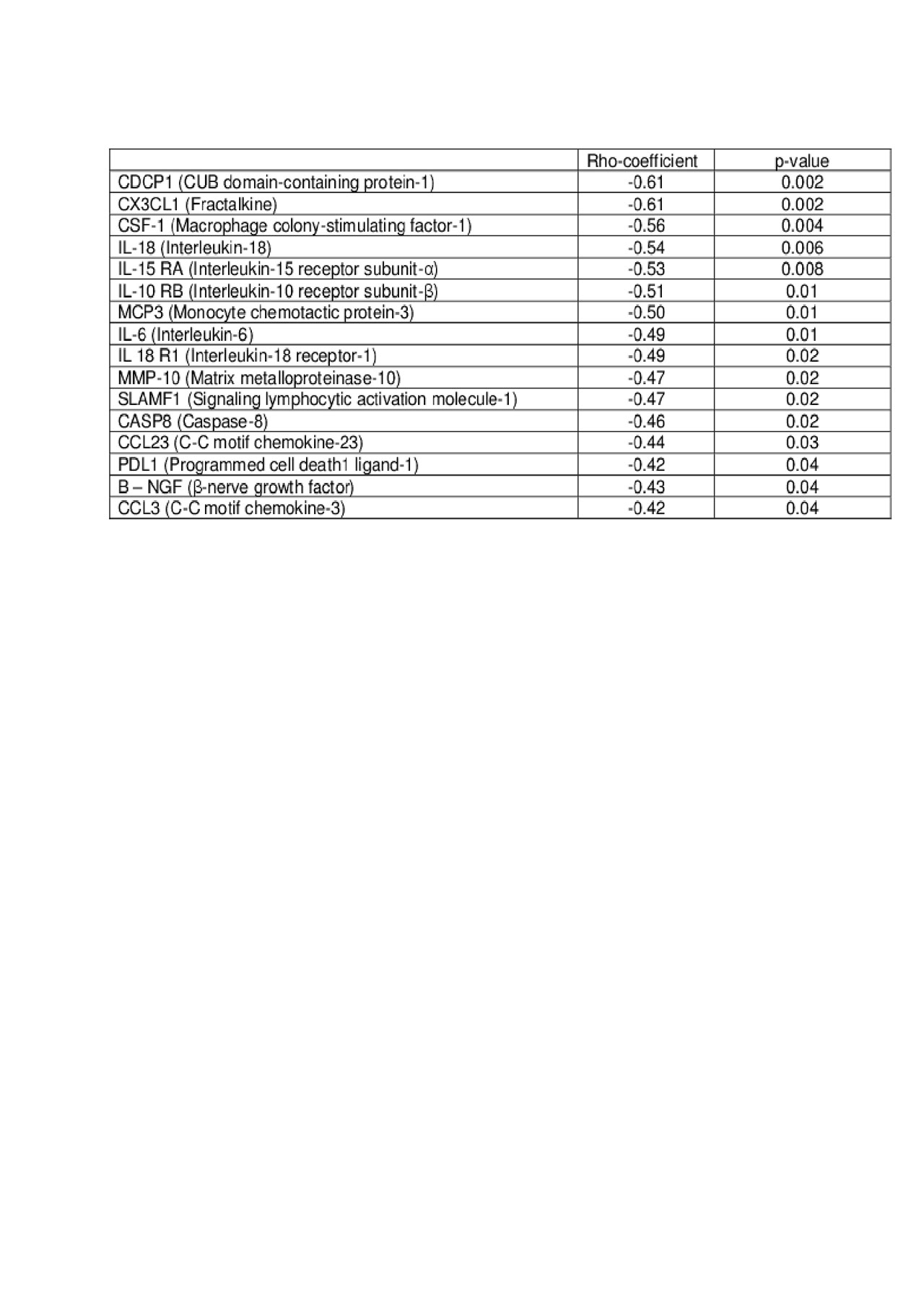
Results: SLE patients have a decreased nocturnal dipping [7% (5 – 13%)], compared to controls [12% (8-20%)] p=0.01. In patients with SLE, lower blood pressure dipping was significantly associated with many inflammatory markers (Table) including CDCP1 (CUB domain-containing protein-1, involved in complement activation), IL15RA (Interleukin-15 receptor subunit-α, which enhances apoptosis), and SLAMF1 (Signaling lymphocytic activation molecule-1, which promotes immunoglobulin production).
Conclusion: Nocturnal blood pressure dipping was less pronounced in patients with SLE compared to control subjects. Lower nocturnal blood pressure dipping was associated with multiple markers of inflammation in patients with SLE.
To cite this abstract in AMA style:
Carranza Leon D, Oeser A, Wu Q, Stein C, Ormseth M, Chung C. Decreased Nocturnal Blood Pressure Dipping in Patients with Systemic Lupus Erythematosus: Association with Markers of Inflammation [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/decreased-nocturnal-blood-pressure-dipping-in-patients-with-systemic-lupus-erythematosus-association-with-markers-of-inflammation/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/decreased-nocturnal-blood-pressure-dipping-in-patients-with-systemic-lupus-erythematosus-association-with-markers-of-inflammation/