Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: To determine whether frailty is associated with patient outcomes 1 year after total hip replacement (THR).
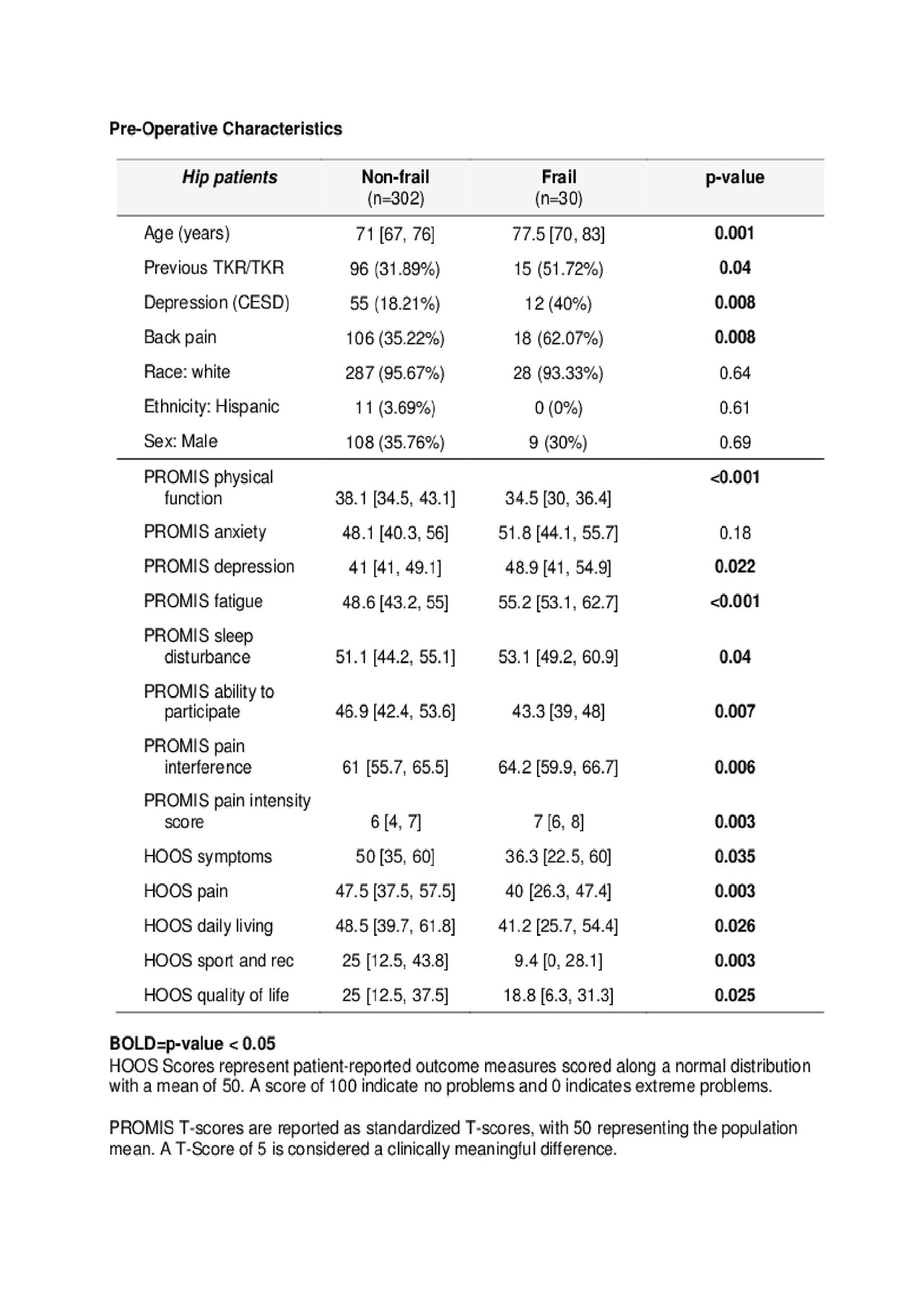
Methods: Patients ≥65yo scheduled for elective primary THR for osteoarthritis were recruited from a musculoskeletal specialty hospital. All were approved for surgery by an internist. Frailty was defined using composite criteria designed for surgical candidates, evaluated at point of care. Hip Injury and Osteoarthritis Outcome Score (HOOS) and PROMIS29 were administered pre-operatively and at 1-year. Depression was measured using the Center for Epidemiologic Studies Depression Scale (CES-D 10). A subset of patients had frailty assessed by their surgeon pre-operatively using the brief, self-report Clinical Frailty Scale for Physicians. Wilcoxon rank-sum and Fisher’s exact tests were used to compare continuous variables and categorical variables, respectively, across frailty status. Multivariable linear and logistic regressions were modeled for each patient-related outcome, adjusting for confounders identified a priori using a directed acyclic graph approach. Spearman correlation coefficients were calculated to evaluate the correlation between frail scales.
Results: 332 hip replacement subjects enrolled, 9% of whom were frail. Frail THR subjects were older, more likely to be depressed, have concurrent back pain, and were also more likely to have had a previous hip or knee replacement. 91.4% provided 1-year follow-up. In a multivariable linear regression controlling for age, gender, race, back pain, education, Charlson comorbidity index, and PROMIS29 anxiety and depression, frailty predicted a clinically meaningful improvement in HOOS pain (β=10.4), which was statistically significant (p=0.01). Frailty also predicted a significant decrease in PROMIS pain interference T-score at 1-year, (β=3.9; p-value 0.023), controlling for the same potential confounders. Frailty did not predict other HOOS subscales or PROMIS29 domains at 1-year. Frailty did not predict cumulative severe adverse events through 1 year or OMERACT-OARSI responder status at 1-year. There was a strong correlation between our frailty definition and the Fried frailty phenotype, (r=0.79; p< 0.001), but a poor correlation with the orthopedic surgeon’s frailty assessment (r=0.16; p=0.78).
Conclusion: Frailty was a strong predictor of less hip-related pain and less overall pain interference 1 year after THR in older adults undergoing elective primary THR. Frailty was not associated with odds of adverse events or OMERACT-OARSI responder status. Surgeon assessment of frailty is not an accurate proxy for the frailty phenotype. Appropriately screened frail patients should not be discouraged from having THR for pain relief, particularly given the known risks of long term NSAIDS and narcotics. These data can aid in surgical decision making for frail patients contemplating THR.
To cite this abstract in AMA style:
Mandl L, Cornell C, Cross M, Gonzalez Della Valle A, Figgie M, Jerabek S, Frey M, Roberts IV J, Do J, Sasaki M, Hupert N, Finik J, Magid S. Frail Patients Have Less Pain After Total Hip Replacement [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/frail-patients-have-less-pain-after-total-hip-replacement/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/frail-patients-have-less-pain-after-total-hip-replacement/