Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose:
Rheumatoid Arthritis (RA) generates high impact on patients and healthcare systems. Adequate control of disease activity depends to a large extent on the access to a Rheumatologist. The type of healthcare system adopted by the governments constitutes a major determinant for the access of patients to an adequate standard of care. Colombia has a contributory and public-subsidized health insurance system, which ensures a universal coverage of the population; however, differences in care access opportunities persist, especially for appointments with sub-specialties. The aim of this study was to compare the disease outcomes of Colombian patients with RA, based on their type of health regime.
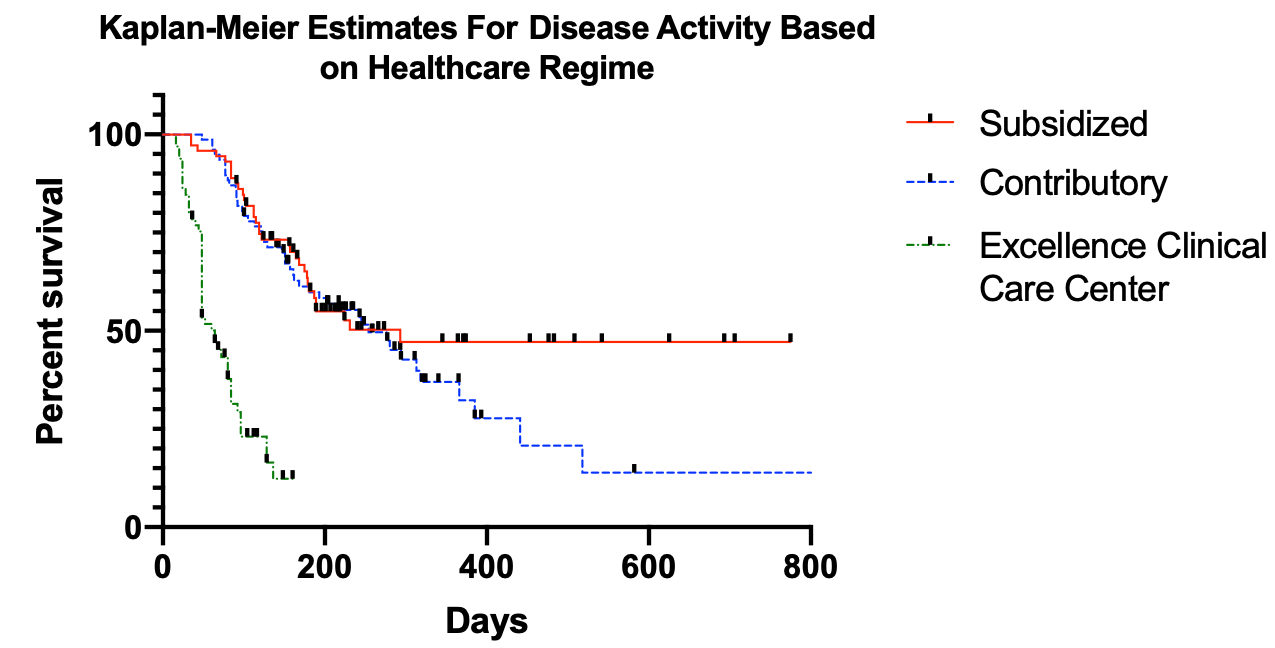
Methods: A retrospective observational study of Colombian patients with RA (Meeting 2010 ACR/EULAR classification criteria), with at least 3 assessments by a rheumatologist, in three outpatient services of different regimes: Contributory (C), Subsidized (S), and an excellence clinical care center (C3). Data collected from clinical records during a follow-up period of 2 years include: age, RA classification, percentage of patients with initial and final high disease activity based on DAS-28 ESR, number of appointments, days between appointments (ordered and real), number of appointments accomplished on time, adherence to treatment, and percentage of time in high disease activity. Mean and 95% confidence intervals were calculated. Statistical differences were calculated using X2 or Kruskal-Wallis test and adjusted for multiple comparisons using the Bonferroni test, with a significance level of p< 0,005. Survival analysis for the achievement of remission/low disease activity during follow-up was developed. Mantel-Cox test was calculated to compare the survival curves for every regime.
Results: A total of 240 patients were included (80 patients per regime). Results are summarized in Table 1. Mean initial age was 53.7 years; 21.6% of patients were men; 79.6% of patients had established RA; 72.9% of patients had initial high disease activity; Mean percentage of time in high disease activity during follow-up was lower in C3 (44.9%), and higher in C (69.1%). At the end of the follow-up, S group had the highest proportion of patients remaining with high disease activity, and C3 the lowest. Survival curve analysis based on Mantel-Cox shows no significant difference between S and C groups (p=0.2903), but were significantly different compared to C3 group (p< 0.0001). Median survival in high disease activity was greater in the S group (293 days), followed by C (254 days), and finally by C3 (64 days).
Conclusion:
Patients treated in the clinical care center had better outcomes based on higher adherence and lower disease activity scores, compared to the other regimes, especially those on Subsidized regime. The type of healthcare regime a patient has access to, is a major determinant of the disease outcomes, specially for chronic diseases in which the success of the treatment depends on a strict follow-up by a specialist. This differences in the access and outcomes are reflected in higher expenses for healthcare system, derived from complications and disabilities that patients could suffer, secondary to inadequate control of the disease.
To cite this abstract in AMA style:
Barahona-Correa J, Florez J, Rodriguez M, Ramirez K, Mendez-Patarroyo P, Coral-Alvarado P, Quintana-López G. Differences in Clinical Outcomes According to the Healthcare Regime in Colombian Patients with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/differences-in-clinical-outcomes-according-to-the-healthcare-regime-in-colombian-patients-with-rheumatoid-arthritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/differences-in-clinical-outcomes-according-to-the-healthcare-regime-in-colombian-patients-with-rheumatoid-arthritis/