Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Symptomatic knee OA is a debilitating condition that affects 14 million adults in the US. We estimated the variability of lifetime OA-related direct and productivity costs as a function of pain and structural severity at presentation to care.
Methods: We used the Osteoarthritis Policy Model, a validated computer microsimulation of knee OA, to evaluate utilization of alternative treatment modalities and lifetime medical and productivity cost for individuals diagnosed with symptomatic and radiographic OA of Kellgren-Lawrence (KL) grade 2, 3, or 4 in moderate (mean 25) or severe (mean 55 ) pain on the Western Ontario and McMaster Universities Osteoarthritis Index pain scale (0-100, 100 is worst) at the time of presentation for OA care. The combinations of three radiographic grades and two pain categories yielded 6 cohorts. To determine the age of presentation to care for each cohort we used additional model runs, coupled with the national data on incidence and structural progression of knee OA. Treatments under consideration included NSAIDs, physical therapy, braces, corticosteroid injections, tramadol, strong opioids (e.g. oxycodone, hydromorphone, hydrocodone, morphine), and total knee replacement. We followed subjects from presentation to OA care until death. Direct medical costs of knee OA treatments were derived from Redbook Online and Medicare reimbursement data. The economic burden of OA was portrayed as the time cost of lost productivity and the societal costs associated with opioid use. Treatment efficacy and opioid-related costs were derived from published literature. Costs were discounted at 3% annually.
Results: Pain severity was the key driver of lifetime time OA-attributable costs, with severe pain adding about $8,000, increasing the discounted direct medical costs by 35% compared to moderate pain across all KL levels considered (Figure). Across all six cohorts, TKR was the largest contributor to the direct medical OA-related cost. The largest contributor to indirect cost was lost work productivity due to OA. The indirect costs comprised between 30%-45% of total (direct plus indirect) OA-attributable costs, ranging from $4,000-$5,000 for those in moderate pain to $8,000-$10,000 among those in severe pain. The percent of patients using strong opioids ranged from 10% (KL 4, severe pain) to 76% (KL 2, severe pain), and the average duration of opioids use ranged from 1.9 (KL 4, severe pain) to 2.7 years (KL 2, moderate pain). The percent of patients receiving TKR ranged from 40% among those followed from diagnosis with KL 2, moderate pain to 82% among those followed from the time they had been diagnosed with KL 4, severe pain. The average age of surgery ranged from 65 to 69 years depending on symptoms and structural severity.
Conclusion: Pain severity at presentation had much greater impact on medical and societal costs than structural severity at presentation. Indirect medical costs comprised between 29% and 44% of total medical OA-attributable costs. These data could be used by policy makers and payers to direct resources toward pain management and optimizing productivity among knee OA patients in the workforce.
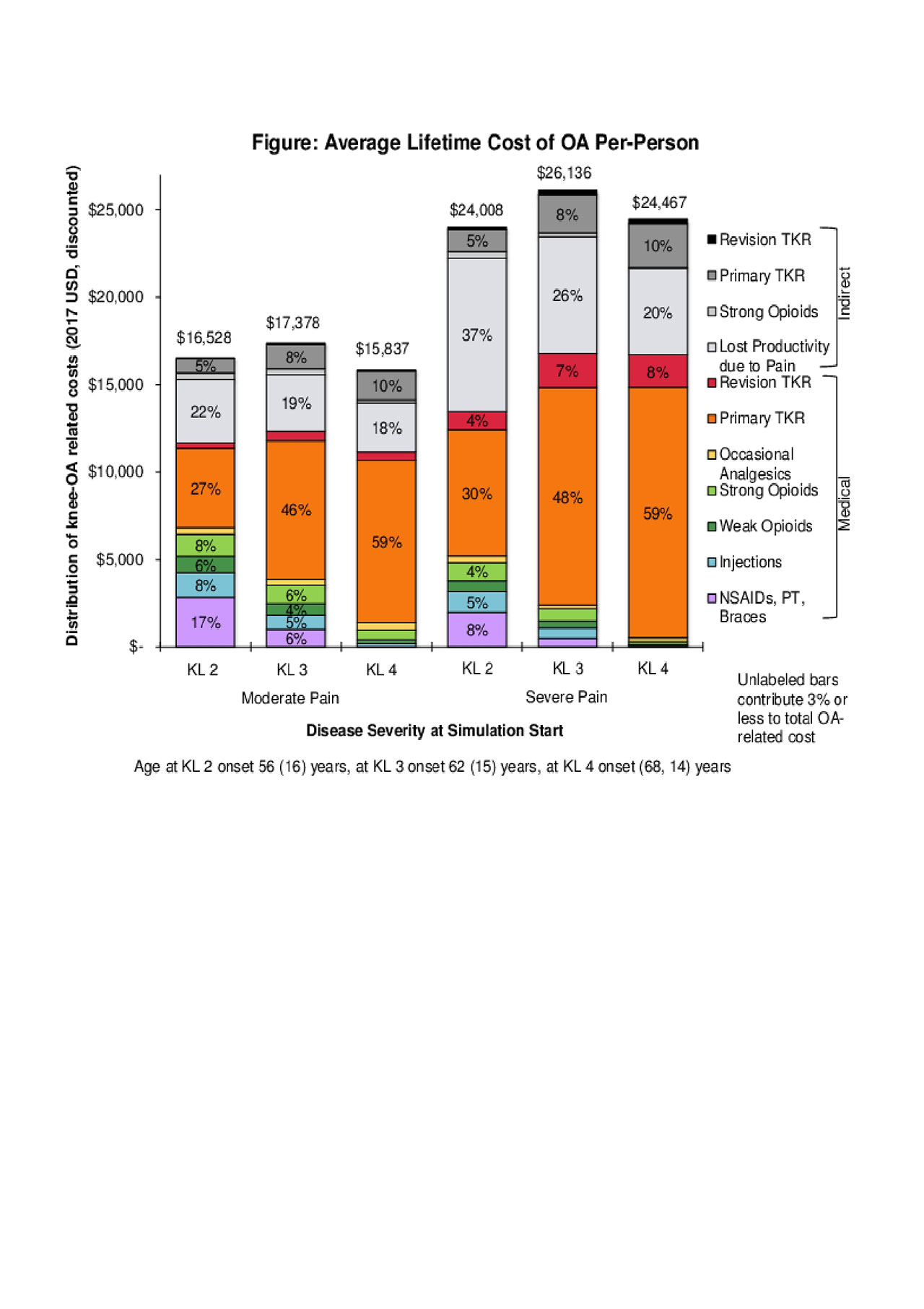
ACR_2019_CostUtilization_figure
To cite this abstract in AMA style:
Stanley E, Sullivan J, Huizinga J, Collins J, Katz J, Losina E. Lifetime Direct Medical and Indirect Cost of Knee Osteoarthritis: Impact of Pain and Structural Severity [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/lifetime-direct-medical-and-indirect-cost-of-knee-osteoarthritis-impact-of-pain-and-structural-severity/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/lifetime-direct-medical-and-indirect-cost-of-knee-osteoarthritis-impact-of-pain-and-structural-severity/
