Session Information
Date: Monday, November 11, 2019
Title: Epidemiology & Public Health Poster II: Spondyloarthritis & Connective Tissue Disease
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Individuals with systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA) often suffer from both acute and chronic pain, and the prevalence of opioid medication use among persons with RA has been estimated at 16%1. Because of the risk of overdose among opioid users, we sought to investigate opioid overdose-related hospitalizations among patients with SLE and RA in comparison to the rest of the population.
Methods: We used the National Inpatient Sample (NIS), which after weighting provides annual estimates for more than 35 million hospitalizations in the US. Analysis was limited to individuals without missing relevant variables hospitalized in 2016. Admissions with opioid overdose were identified based on these ICD-10-CM codes: T40.0-40.4, T40.6, X42.x, X62.x or Y12.x, which could be included as the primary reason for admission or one of up to 30 causes. SLE and RA were also captured in ICD-10-CM codes (M32.1x, M32.8, M32.9 and M05.x, M06.0x, M06.2x, M06.8x, M06.9, M08.x respectively); patients with codes for both conditions were classified as SLE. We compared the proportion of opioid overdose admissions among patients with SLE, RA, and neither condition using chi-squared tests. We used Poisson regression to model admissions due to opioid overdose as a function of disease (SLE, RA, or neither), controlling for demographics (age, sex, race) and socioeconomic status (SES) characteristics (health insurance and residence in a low-income ZIP code). All analyses accounted for the complex sampling design of the NIS.
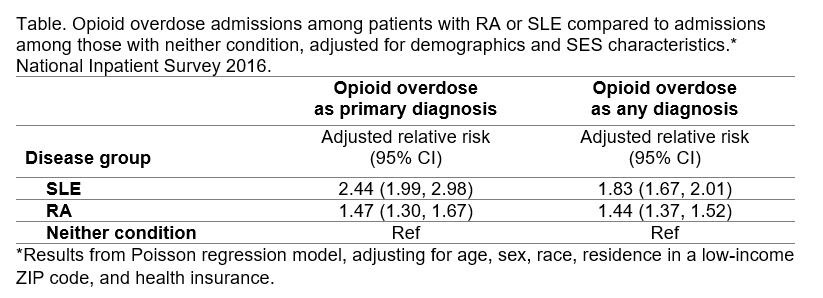
Results: Among 33,207,455 hospitalizations in 2016 included in the analysis, 512,740 (1.5%) were of patients with RA and 147,480 (0.44%) with SLE. A higher proportion of hospitalizations were due to opioid overdose as a primary cause among patients with RA (0.23%) or SLE (0.34%), in comparison to patients with neither condition (0.17%; p < 0.01). Including all diagnoses of opioid overdose increased the proportions to 1.46% for patients with RA, 1.50% for SLE, and 0.85% for those with neither condition, and the differences were still significant (p < 0.01). After accounting for demographic and SES characteristics of the hospitalized patients, both RA and SLE were associated with higher relative risks of opioid overdose hospitalizations compared to patients with neither condition, either as a primary diagnosis or any diagnosis. SLE was associated with a higher relative risk of opioid overdose hospitalization compared to RA (Table).
Conclusion: RA and SLE were associated with a 1.5 to 2-fold higher risk of opioid overdose hospitalization compared to the general population. Local and national overdose intervention programs should consider targeting RA and SLE individuals as at potentially increased risk for opioid overdose.
Reference:
1. Lee YC, Kremer J, Guan H, Greenberg J, Solomon DH. Chronic Opioid Use in Rheumatoid Arthritis: Prevalence and Predictors. Arthritis Rheumatol. 2019 May;71(5):670-677.
To cite this abstract in AMA style:
Anastasiou C, Li J, Trupin L, Schmajuk G, Yazdany J. Opioid Overdose Hospitalizations in Patients with Systemic Lupus Erythematosus and Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/opioid-overdose-hospitalizations-in-patients-with-systemic-lupus-erythematosus-and-rheumatoid-arthritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/opioid-overdose-hospitalizations-in-patients-with-systemic-lupus-erythematosus-and-rheumatoid-arthritis/