Session Information
Date: Sunday, November 10, 2019
Title: 3S089: Health Services Research I: Clinical Perspectives (951–956)
Session Type: ACR/ARP Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Psychiatric comorbidity is increased in rheumatoid arthritis (RA) and may complicate medical care, increasing the risk of adverse health outcomes and health care utilization (HCU). We describe the impact of psychiatric comorbidity in RA on HCU (ambulatory care visits, hospitalizations, number of hospital days, prescription drugs) including recommended preventive health care (influenza vaccination, pap and mammogram tests).
Methods: We accessed administrative health data (1984-2016) from a region with near universal health coverage and identified a prevalent cohort with diagnosed RA (n=16975). We matched each RA case on age and sex with up to 5 controls (CNT) with no RA diagnosis (n= 84756). Psychiatric morbidities including depression, anxiety and bipolar disorder (PsyMb) were identified in RA cases and CNT. Annual rates of ambulatory care visits [mean visits (SD)/person], all-cause hospitalization (%), days of hospitalization [(mean days (SD)/hospitalization], total prescribed drugs (mean (SD)/person), influenza vaccination (%), pap tests (%), and mammograms (%), were age and sex-standardized to the 2010 Canadian population. Ambulatory care visits were categorized by provider (family physician [FP], rheumatologist, mental health specialist, other specialist). We compared rates of HCU and preventive care amongst four groups (CNT, CNT+PsyMb, RA, RA+PsyMb) using generalized linear models adjusted for age, sex, rural vs urban residence, income quintile, total comorbidities (assessed by John Hopkins Aggregated Diagnostic Groups), DMARD prescription, and RA-specific procedures (e.g. arthroplasty). Rates and percentages are reported with 95% confidence intervals (CI). We tested whether PsyMB and RA had additive or synergistic effects on HCU or preventive care.
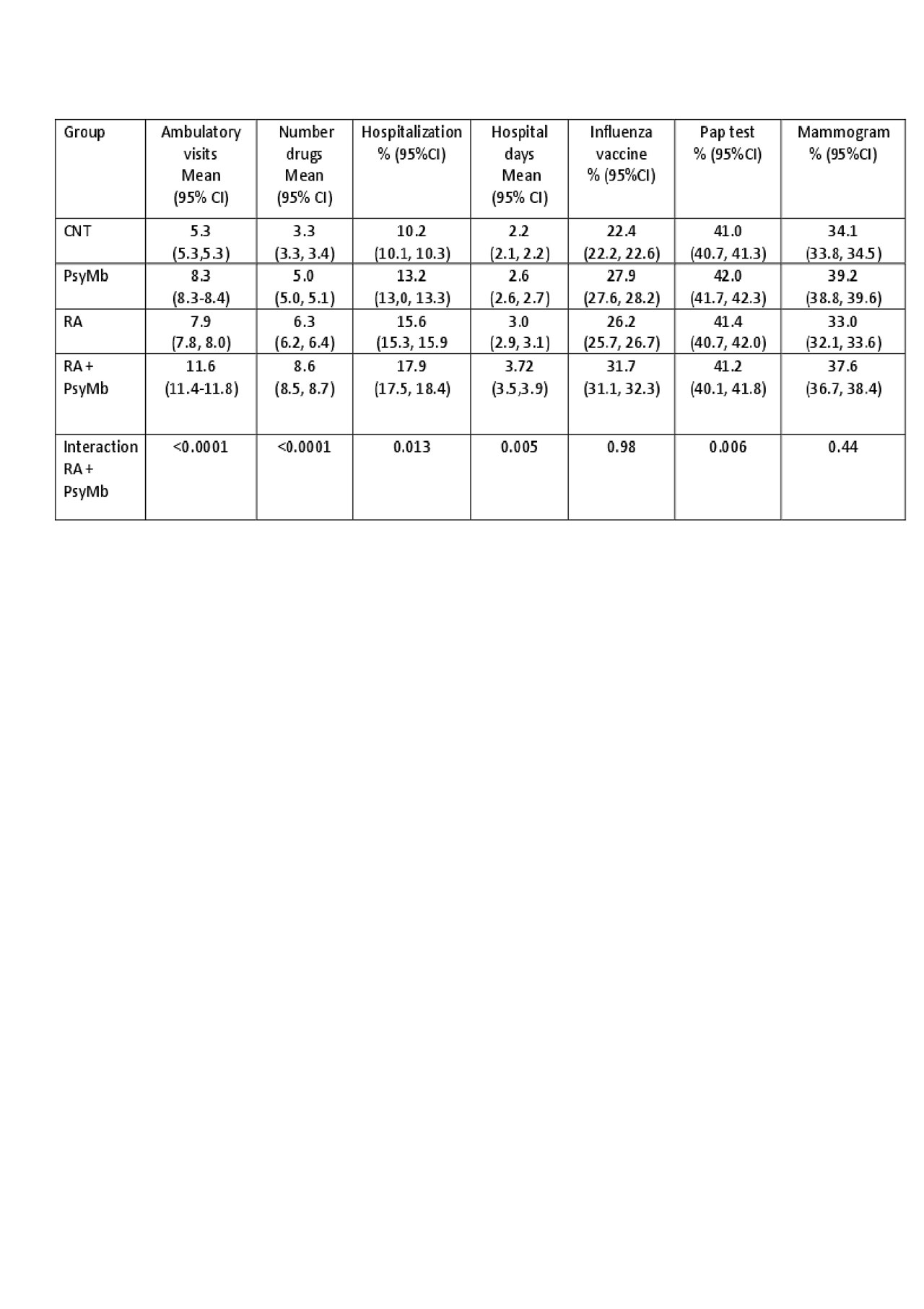
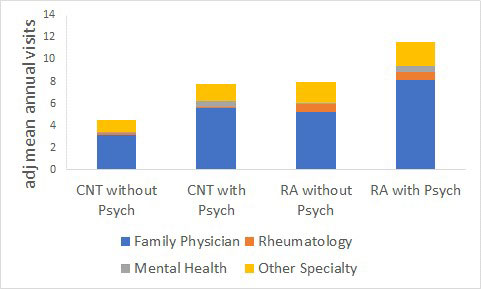
Results: Most RA patients were female (72%) and urban residents (59%). Mean age at diagnosis was 54(SD:16) years. Mean follow-up duration was 13(SD:9) years. After adjustment, compared to RA without PsyMb, those RA with PsyMb had an additional 3.7 (95%CI: 3.5-3.9, p< 0.0001) ambulatory visits/year, 2.3% (95%CI: 1.8-2.8; p< 0.0001) increased hospitalization, 0.7 (95%CI: 0.5-0.95 p< 0.0001) more hospital days/admission and were prescribed 2.3 (95%CI 2.2-2.5; p< 0.0001) more drugs (Table). RA+PsyMb had increased ambulatory care visits for all providers particularly FPs [additional 2.9 FP visits/year (2.8, 3.0); interaction between RA, Psych and provider p< 0.0001] (Figure). Overall rates of preventive care in RA were 34% for influenza vaccination, 38.3% for mammograms and 43.3% for pap tests when indicated. RA+PsyMb had increased influenza vaccinations (5.5%; 4.8-6.2%, p< 0.0001) and screening mammograms (4.7%; 3.7-5.7%, p< 0.0001) but not pap tests (0.2%; -1-0.06%, p=0.6). No interactive effects were significant for influenza vaccination or mammogram preventive measures between RA and RA+PsyMb (Table).
Conclusion: Psychiatric comorbidity increases health care utilization among those with RA, particularly for FP visits. Increased contact with care providers may contribute to higher rates of some preventative care such as vaccination, but overall preventive care rates remained suboptimal.
To cite this abstract in AMA style:
Hitchon C, Bernstein C, Bolton J, El-Gabalawy R, Fisk J, Katz A, Lix L, Marriott J, Patten S, Peschken C, Sareen J, Singer A, Walld R, Marrie R. The Impact of Psychiatric Comorbidity on Health Care Utilization and Preventive Health Care in Rheumatoid Arthritis: A Population Based Study [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/the-impact-of-psychiatric-comorbidity-on-health-care-utilization-and-preventive-health-care-in-rheumatoid-arthritis-a-population-based-study/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-impact-of-psychiatric-comorbidity-on-health-care-utilization-and-preventive-health-care-in-rheumatoid-arthritis-a-population-based-study/