Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose:
Many RA patients have variable disease activity over time due to disease variability, reduction in efficacy of current medications, environmental factors and other co-morbid disease changes. Prior methodologies have been developed but in the absence of application with real data the models have not been validated. The model applied to patient clinical data may potentially provide insights into clinically relevant associations to disease state transitions and enhance treatment methods.
Methods:
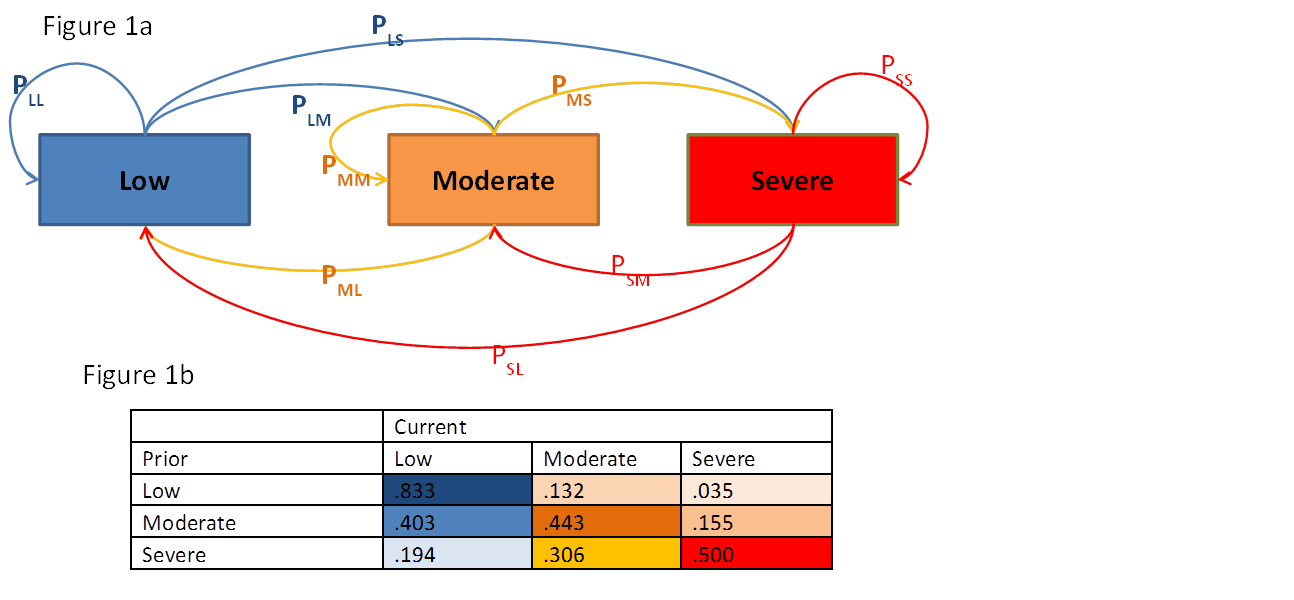
Disease activity states of low, moderate and severe were defined using CDAI (Low: CDAI≤10; Moderate 10
Estimated transition probabilities in the population are in Figure 1b, showing that if the disease state at the prior visit was low then the probability of remaining low (PLL) is 0.833 and the probability of transitioning to moderate disease (PLM) at the next visit is .132, and to severe (PLS) is .035. Transition from any state to low disease was seen to improve from 2001-05 to 2009-12 with PLL going from 0.79 to 0.84 (p<0.001). Logit models estimated the effect of covariates adjusted for time between visits. A patient in a prior state of moderate disease had a relative risk ratio of 7.6 (95%CI: 7.08-8.21) to be in moderate disease at the current visit (vs a patient in a prior state of low disease) if no DMARD was initiated on the prior visit. If a DMARD was initiated the risk was reduced to 4.08 (3.59-4.63). Longer duration of RA increased the risk of transition in a moderate or severe state. Age and insurance did not interact with prior disease states but showed an association with current disease state – with private insurance associated with lower levels of disease and age 50-64 with a larger risk for moderate and severe disease vs age <50.
Conclusion:
Estimation of transition probabilities among disease states provides a snapshot of RA population risks dependent upon prior states and a methodology for examining factors associated with those risks. Current models estimate the impact of initiating DMARDS and the duration of RA and provide a proof of concept of the modeling framework that can be mined for examining further associations.
Disclosure:
G. W. Reed,
Corrona,
2,
University of Massachusetts Medical School,
3,
Corrona,
5,
Harvard Medical School,
;
D. H. Collier,
Amgen Inc.,
1,
Amgen Inc.,
3;
A. S. Koenig,
Pfizer Inc,
3,
Pfizer Inc,
1;
K. C. Saunders,
Corrona,
3;
J. M. Kremer,
Bristol-Myers Squibb, Genentech, Pfizer, HGS, UCB,
2,
Amgen, Abbott, Genentech, Pfizer ,
5,
Amgen, Abbott, BMS,
8,
Corrona,
4;
S. Kotak,
Pfizer Inc,
1,
Pfizer Inc,
3.
« Back to 2012 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/transitions-among-disease-activity-states-estimates-and-models-of-covariate-associations/