Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Ankylosing spondylitis (AS) is an inflammatory arthritis that predominantly affects the axial skeleton, but commonly affects peripheral joints as well. Peripheral joint involvement often leads to total hip arthroplasty (THA) or total knee arthroplasty (TKA) in AS. We evaluated the relation of tumor necrosis factor inhibitors (TNFi) and other therapies in AS relative to nonsteroidal anti-inflammatory drugs (NSAIDs) to the risk of THA/TKA.
Methods: We conducted a nested case control study using 1994-2018 data from the OptumLabs® Data Warehouse, which includes medical and pharmacy claims, laboratory results, and enrollment records for commercial and Medicare Advantage enrollees. The database contains longitudinal health information on enrollees and patients, representing a diverse mixture of ages, ethnicities and geographical regions across the United States. Claims were used to identify patients with AS ages 18-89. Subjects were required to have medical and pharmacy coverage at least 6 months prior to AS diagnosis. Incident THA/TKAs were defined by diagnostic codes. THA or TKA cases were matched to four controls by sex, age (+/- 3 years), AS diagnosis year (+/- 1) and insurance type (private or Medicare). We assessed AS treatment in 6-month period prior to THA or TKA, using categories of NSAID (referent), symptom modifying anti-rheumatic drug (SMARD), and TNFi, either alone or in combination with other therapies. We evaluated the relation of each type of treatment to risk of THA or TKA using conditional logistical regression, with adjustment for age and history of chronic kidney disease, diabetes, liver disease, obesity, and peptic ulcer disease at baseline. Sensitivity analyses included 3-month and 14-month exposure assessment periods and models assessing THA and TKA separately.
Results: Among 22,166 adults with AS meeting eligibility criteria, we identified 539 cases of THA or TKA, and 1568 matched controls. Mean age was 58.9 (SD +/- 11.2) years, and 51.5% were female. Relative to NSAID use, the adjusted OR (aOR) within the 6-month exposure assessment period for TNFi only use was 0.45 (95% CI 0.26-0.78) and the aOR for SMARD only use was 0.49 (95% CI 0.32-0.75; see Table). Associations for other combinations of therapies were not significant. Sensitivity analyses using 3-month and 14-month exposure assessment periods yielded aORs for TNFi only use of 0.39 (95% CI 0.22-0.69) and 0.44 (95% CI 0.23-0.86), respectively, and for SMARD only use aORs of 0.55 (95% CI 0.35-0.84) and 0.56 (95% CI 0.37-0.84). Results were similar for analyses of THA and TKA individually.
Conclusion: In this large sample of US adults with AS, the use of TNFi only and SMARD only were associated with lower odds of THA and TKA relative to NSAID use alone. Combinations of AS therapies were not associated with lower odds of THA and TKA. SMARD or TNFi therapy appear to have beneficial effects beyond the spine in AS on peripheral joints compared with NSAIDs; however, whether this may reflect benefits of those therapies versus detrimental effects of NSAIDs cannot be discerned.
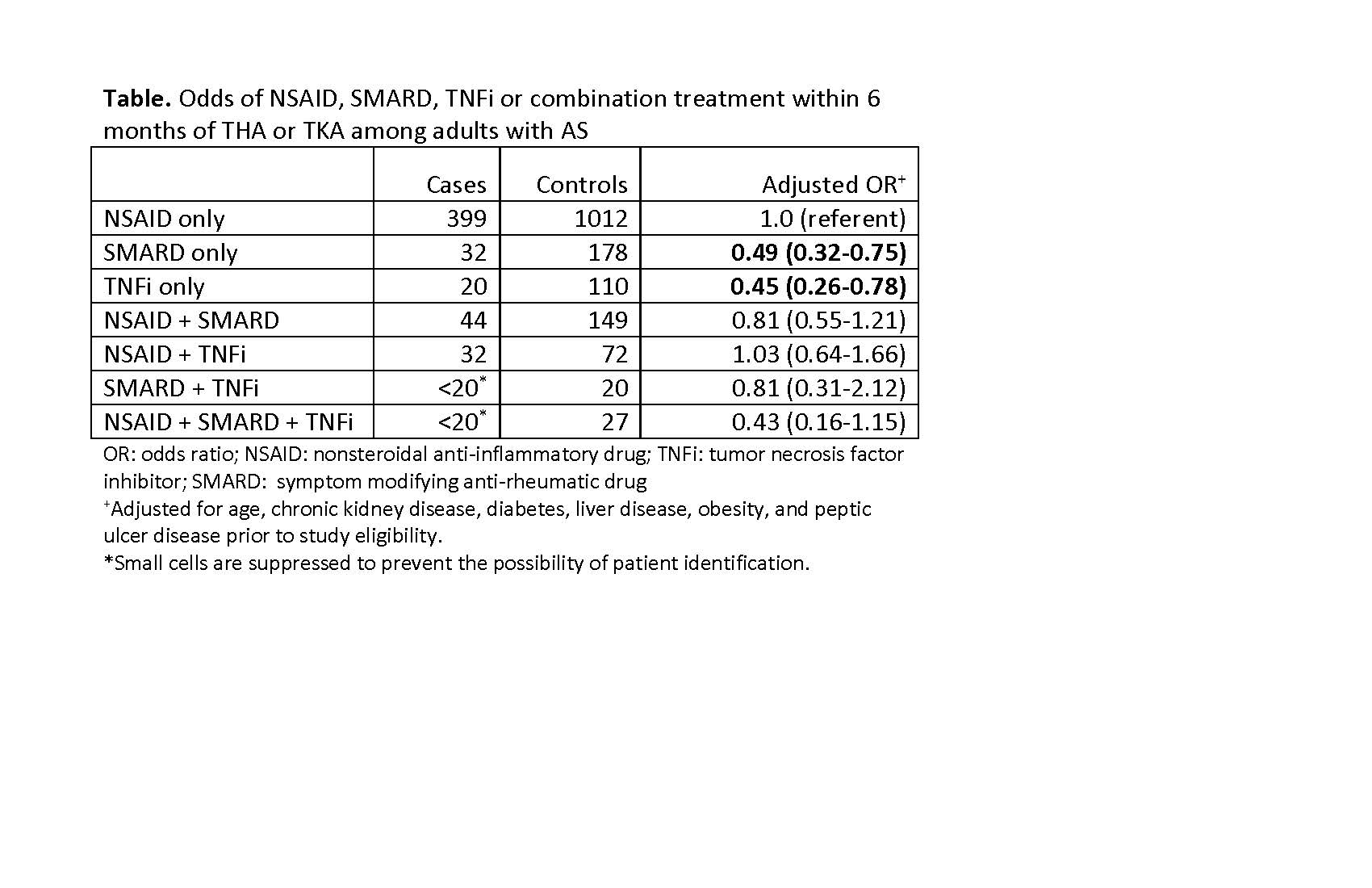
Table.ForACRAbstract.Updated06032019
To cite this abstract in AMA style:
Stovall R, Peloquin C, Felson D, Neogi T, Dubreuil M. Relation of Therapies for Ankylosing Spondylitis to Risk of Total Hip and Knee Arthroplasty [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/relation-of-therapies-for-ankylosing-spondylitis-to-risk-of-total-hip-and-knee-arthroplasty/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/relation-of-therapies-for-ankylosing-spondylitis-to-risk-of-total-hip-and-knee-arthroplasty/
