Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose:
While medication persistence can act as a substitute metric for effectiveness, few studies have examined real-world patterns of bDMARD persistence by line of treatment and by patient-reported reasons for discontinuation in patients with RA.
Methods: From 2006 to 2018, participants with RA in FORWARD, The National Databank for Rheumatic Diseases, a US-wide observational longitudinal study, reported medication use and reasons for discontinuation. Discontinuation was defined as stopping the use of biologic medications for RA or adding another DMARD. We determined discontinuation rates of individual bDMARD initiators and grouped by action mechanism, delivery method, previous bDMARD history, concomitant use of csDMARDs such as methotrexate and prednisone and self-reported reasons for discontinuation. The latter were randomly assigned when more than 1 reason was given. Propensity score (PS) analyses were conducted overall and by line of treatment, defined as the conditional probability of being treated with TNF or Non-TNF (NTNF). The goal was to remove the baseline characteristics of patients being assigned to one of the two treatments and reduce the channeling bias. Propensity scores were calculated using a logistic regression with treatment (TNF vs NTNF) as dependent variables and several independent variables used as adjustments in the Cox models to evaluate drug survival.
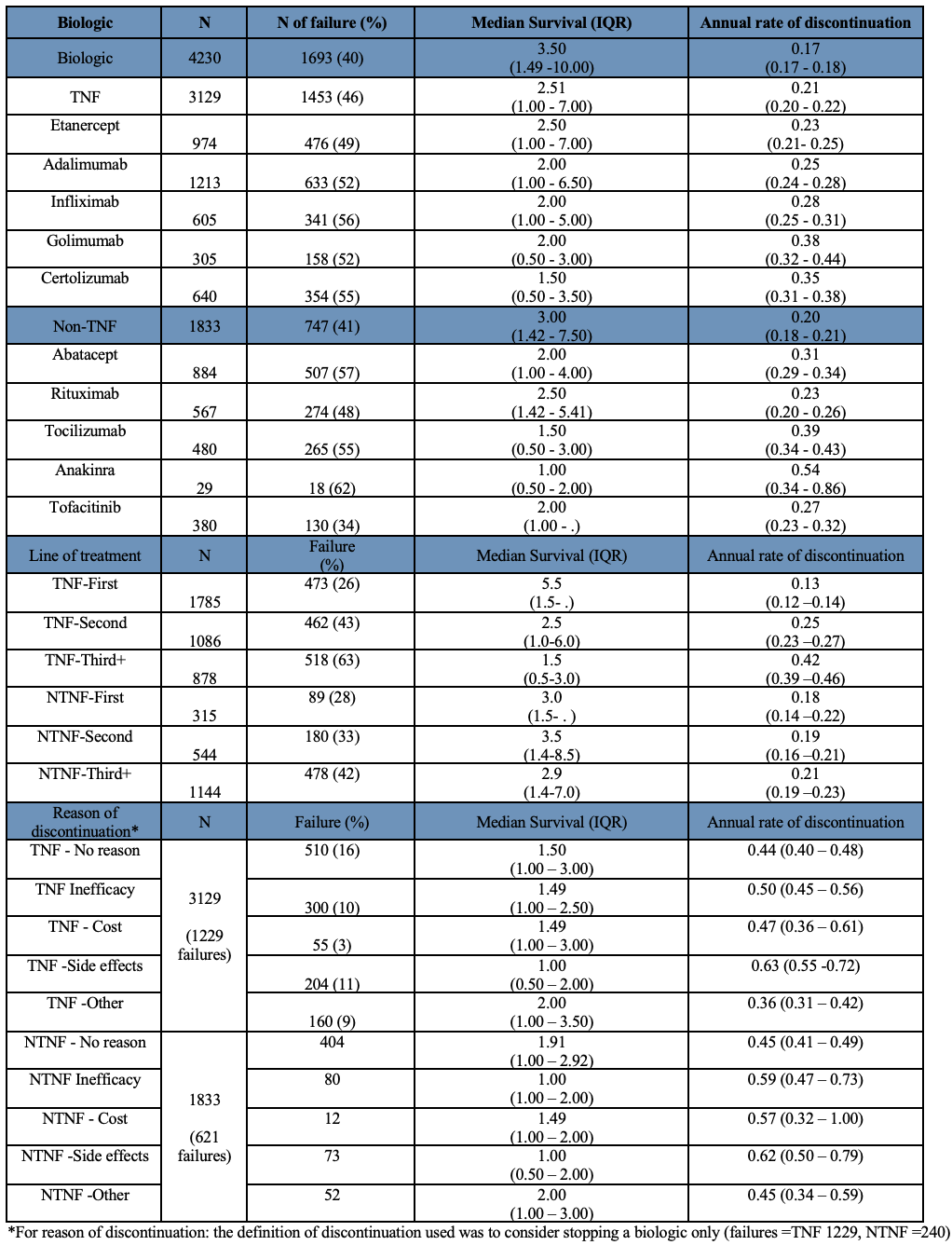
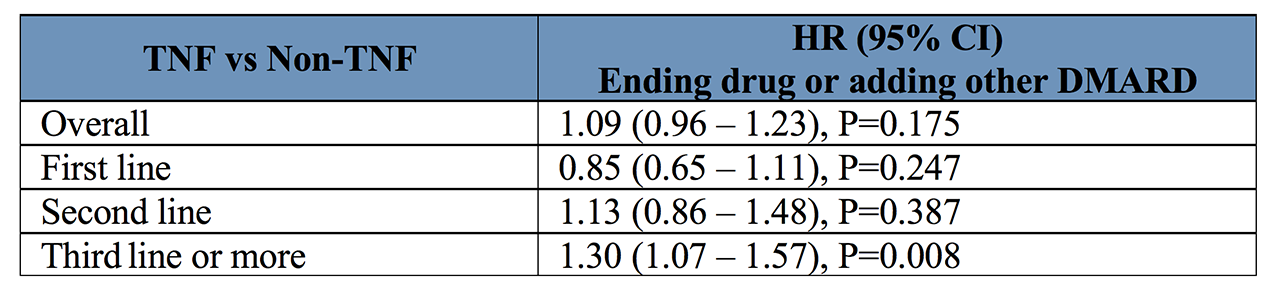
Results: Strict inclusion criteria requiring an observation before and after bDMARD initiation resulted in 4,230 RA patients studied, 3129 initiating a TNF and 1833 initiating NTNF bDMARD or tsDMARD. Mean age of patients was 58 years with a median RA duration of 16 years. TNF had annual discontinuation rates of 0.13 (0.12-0.14) as first line, 0.25 (0.23-0.27) as second line, and 0.42 (0.39-0.46) as third line treatment. NTNF bDMARDs and tsDMARDs showed discontinuation rates of 0.18 (0.14-0.22) per year as first line bDMARD, 0.19 (0.16-0.21) as second line, and 0.21 (0.19-0.23) as third line (see Table 1 for more details). By line of treatment, TNF had lower discontinuation rates used as a 1st line medication compared to NTNF bDMARDs and tsDMARDS, which showed similar persistence regardless of treatment line. However, after adjustment for baseline characteristics through the PS analyses (see Table 2) in the comparison of TNF vs NTNF, only 3rd line treatment showed a difference with TNFs having an 30% increased likelihood of discontinuing compared with NTNF patients. Importantly, long-term persistence was similar for TNF and non-TNF overall. Side effects followed by inefficacy were the most frequent reasons for discontinuation for both action mechanisms (see Figure 1). Cost was also a significant reason among NTNF patients.
Conclusion: While our findings showed relatively low discontinuation rates, the more recently-available non-TNF bDMARDs had similar rates as TNF after propensity score adjustment, which aligns with the latest ACR RA treatment guidelines. With additional follow-up, similar analyses should be done with jakinibs.
To cite this abstract in AMA style:
Grinnell M, Pedro S, Michaud K. Factors Influencing Discontinuation in Long-term RA Treatment [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/factors-influencing-discontinuation-in-long-term-ra-treatment/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/factors-influencing-discontinuation-in-long-term-ra-treatment/