Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Gout is one of the most common inflammatory arthropathies. Despite available urate lowering therapies (ULT), many patients progress to chronic or advanced gout, characterized by the development of tophi, chronic inflammatory arthritis, and other manifestations resulting from persistent urate deposition. Although numerous guidelines exist for the management of gout, there is little information on the frequency of their implementation in the medical community.
The objective of this research was to evaluate the real-world practice patterns in patients diagnosed with gout using a large administrative claims database from the United States.
Methods: We carried out a retrospective analysis to identify patients with gout over an approximately 6-year period from October 2012 to August 2018. This study used data from the Symphony Integrated Dataverse, an administrative database covering over 250 million patients across the United States. Patients were identified as having gout if they were >18 years of age and had at least two medical claims for the diagnosis of gout on different days, separated by at least 3 months. Patients with acute gout were identified by ICD-10 code M10.*, chronic non-tophaceous gout (M1A.***0), tophaceous gout (M1A.***1) and uncontrolled gout (M10.*, M1A.*), the latter manifested by three gout codes (any) in the primary diagnosis position and three urate tests within the same calendar year. Percent and frequency of urate testing, rheumatology specialist visits, and prescriptions for ULT (allopurinol, febuxostat, probenecid, and lesinurad) were evaluated for each diagnostic group.
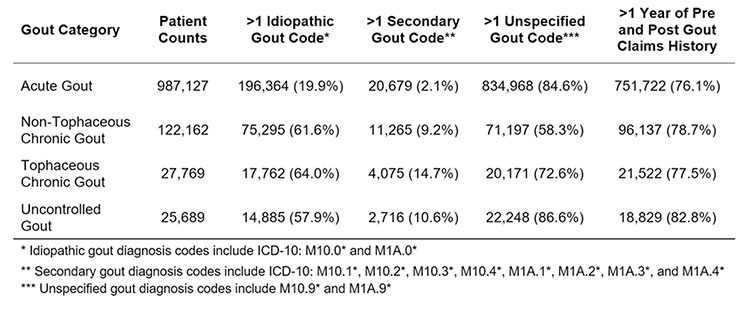
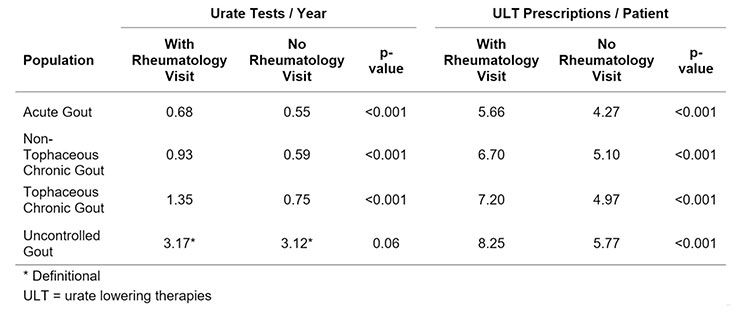
Results: We identified 1,162,747 gout patients (Table 1). The median age was 63 (range: 19-80), 74.1% were male, and the average duration of claims history in the database was 5.6 years. As shown in Figure 1, gout patients were seen most frequently by internists and family medicine practitioners. Patients with acute gout were infrequently see by rheumatologists, but the likelihood of encountering a rheumatologist progressively increased in subjects with advanced gout (chronic nontophaceous< tophaceous=uncontrolled). In all groups, the frequency of serum urate testing and receipt of a prescription for ULT significantly increased in gout patients seen by a rheumatologist (Table 2).
Conclusion: Most subjects with acute gout are not seen by a rheumatologist and less than half of those with advanced gout encounter a rheumatologist. However, measurement of serum urate and prescriptions for ULT are more frequent in those seen by a rheumatologist, but measurement of serum urate and prescriptions of ULT are not uniform. More frequent referral to rheumatologists and closer adherence to guidelines may improve outcomes for gout patients.
To cite this abstract in AMA style:
Edwards N, Schlesinger N, Clark S, Paige J, Arndt T, Lipsky P. Gout Management in the Medical Community: A Claims-Based Analysis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/gout-management-in-the-medical-community-a-claims-based-analysis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/gout-management-in-the-medical-community-a-claims-based-analysis/