Session Information
Session Type: Poster Session (Sunday)
Session Time: 9:00AM-11:00AM
Background/Purpose: With the advent of JAK inhibitors has come increased concerns for the risk of venous thromboembolism (VTE), which was already known to be increased in RA due to inflammation. Although it can be potentially a fatal condition, the other adverse outcomes of VTE, particularly the risk of atherosclerotic cardiovascular disease (CVD), are not well-known in RA. As this potential association has clinical implications regarding screening and risk factor modification, we performed a cohort study to determine the risk of subsequent ASCVD in RA patients with unprovoked first VTE.
Methods: RA patients with ≥1 year participation in FORWARD, The National Databank for Rheumatic Diseases, from 1998 through 2018 were assessed for incident nonfatal or fatal ASCVD (myocardial infarction and stroke) validated from hospital/death records. We excluded patients with prior VTE/ASCVD and active cancer. Among these patients, we identified patients with first unprovoked VTE (deep venous thrombosis [DVT] and pulmonary emboli [PE] not associated with cancer, recent surgery, hospitalization, fracture, or pregnancy). We calculated event rates and estimated the risk of subsequent ASCVD in patients with incident VTE compared to patients with no history of VTE and ASCVD by using Cox proportional hazards with adjustment for sociodemographics, comorbidities, and RA severity measures.
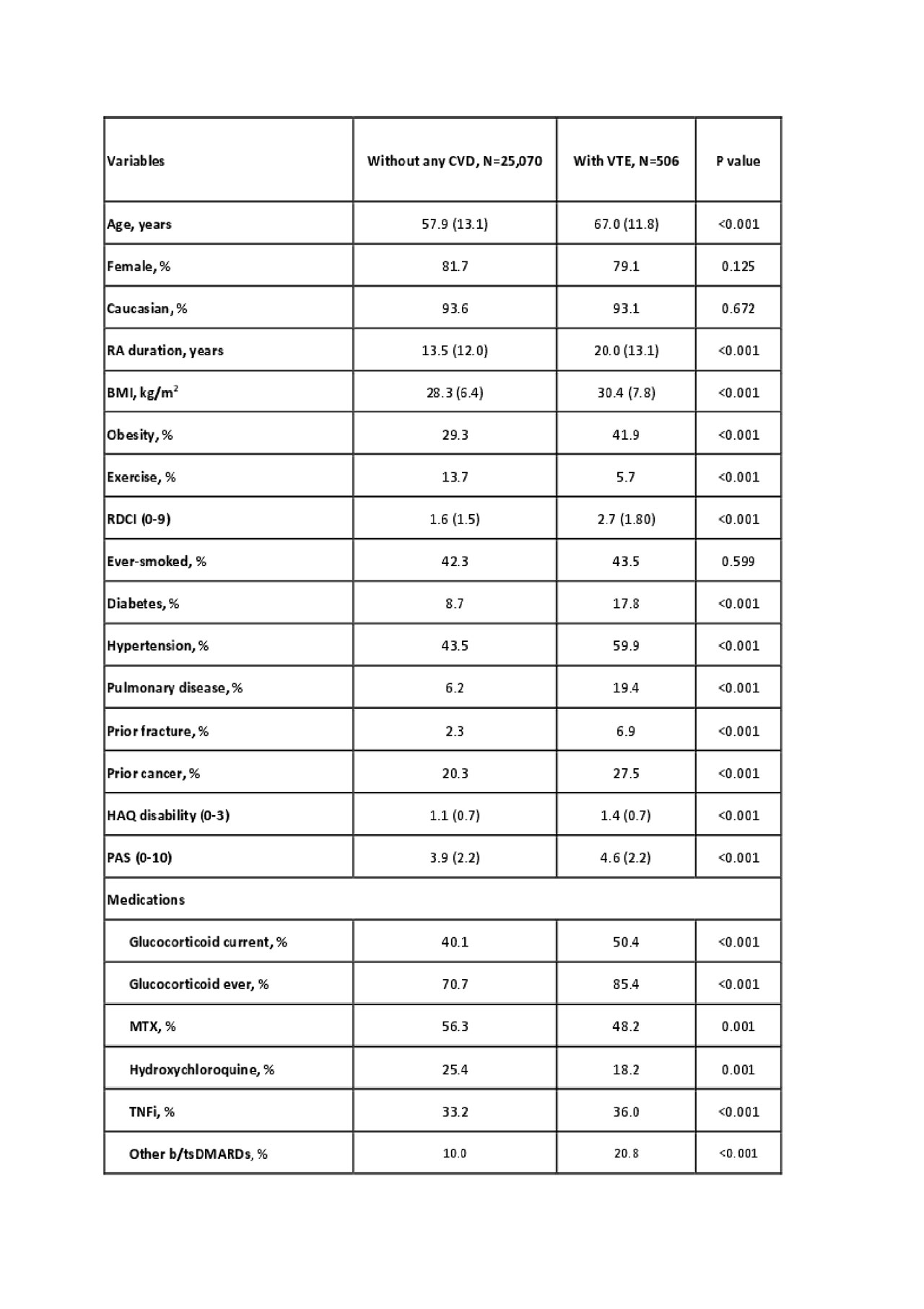
Results: In 25,070 RA patients with no VTE or ASCVD and 506 patients with first unprovoked VTE (without prior ASCVD), we identified 1,283 and 38 first ASCVD events during median (IQR) 4.7 (2.4-8.9) years of follow-up. Baseline characteristics of patients with VTE and without any CVD are presented in Table 1. Patients with unprovoked VTE had worse RA characteristics (disease duration, HAQ, disease activity, glucocorticoid use) and more frequent traditional CV risk factors (diabetes, hypertension, and obesity). The incidence rate (95% CI) of ASCVD was higher in patients with VTE vs. patients without any CVD (8.68 [8.22-9.17] vs. 23.53 [17.12-32.33] per 1,000 patient-years) (Table 2). After multivariable adjustment for baseline differences, we found that patients with an unprovoked VTE had a significantly increased risk of ASCVD (HR [95% CI], 2.05 [1.43-2.95]). The risk increase persisted when we assessed patients with only DVT (HR [95% CI], 1.93 [1.22-3.06]) and the risk in patients with PE was even higher (HR [95% CI], 2.52 [1.57-4.04]) (Table 2).
Conclusion: RA patients with unprovoked VTE as the first CVD, even with only DVT, had twofold risk of ASCVD. Future studies are needed to clarify to what extent chronic inflammation and traditional CV risk factors contribute to this association. Nevertheless, RA patients with unprovoked VTE should be evaluated carefully for ASCVD in the presence of concerning symptoms. Also, more vigilant CV risk screening and treatment should be considered in these patients.
To cite this abstract in AMA style:
Ozen G, Pedro S, Schumacher R, Simon T, Michaud K. Risk of Subsequent Atherosclerotic Cardiovascular Disease After the First Unprovoked Venous Thromboembolism in Patients with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/risk-of-subsequent-atherosclerotic-cardiovascular-disease-after-the-first-unprovoked-venous-thromboembolism-in-patients-with-rheumatoid-arthritis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/risk-of-subsequent-atherosclerotic-cardiovascular-disease-after-the-first-unprovoked-venous-thromboembolism-in-patients-with-rheumatoid-arthritis/