Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with rheumatoid arthritis (RA) have a higher risk of surgical site infection than patients with osteoarthritis (OA). Disease modifying therapy is widely used by RA patients, and biologic medications may increase Staphylococcus aureus colonization rates. Because S. aureus colonization likely increases risk of surgical infection, perioperative assessments and therapies to decrease risk of invasive S.aureus infections may be warranted. The objective of this study was to determine if there was a difference in S. aureus carriage among patients with RA, OA, and RA on biologics (RA+B).
Methods: An a priori power analysis determined 123 participants per group were needed to detect a relative difference of 20% with 80% power. After IRB approval, patients were screened; included patients met ACR classification criteria. Patients were approached between April 2017 and May 2018 and performed a nasal swab using the Center for Disease Control’s swabbing protocol; questionnaires pertaining to health status were collected. Swabs were inoculated onto ChromAgar/ChromID MRSA plates for detection of S. aureus. Mann-Whitney U and Chi-square tests were used to evaluate baseline differences between groups. Logistic regression evaluated the associations between groups and S. aureus carriage. All statistical analyses were performed using SAS Software version 9.3 (SAS Institute, Cary, NC); statistical significance was defined as p<0.05.
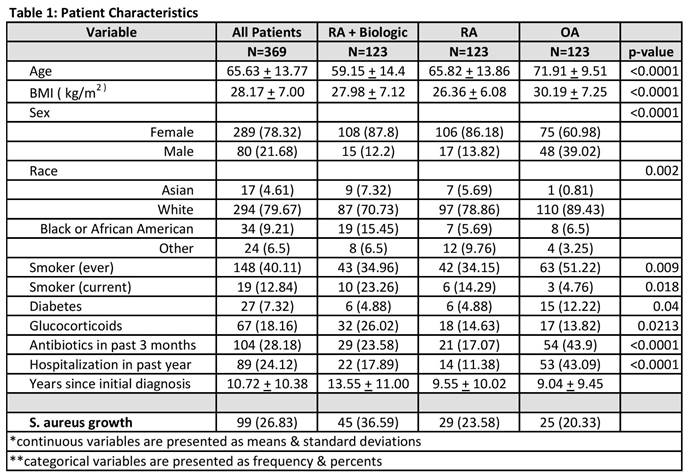
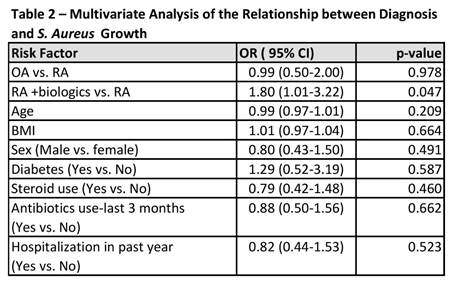
Results: Overall the cohort evaluated had a mean age of 66 (+/-13.7), BMI of 28 (+/-7.0), and were predominantly female (78%) (Table 1). 28% were on antibiotics within three months prior to the swab, 18% were currently on steroids, and 24% had been hospitalized within the last year. We found differences in age (p<0.001), BMI (p<0.001), sex (p<0.001), diabetes (p=0.04), steroid use (p=0.02), antibiotic use (p<0.001), and hospitalizations within the last year (p<0.001). S. aureus carriage was most prevalent in RA+B (37%), followed by RA (24%), and OA (20%). After multivariate adjustment, RA+B was found to have increased odds of S. aureus (OR=1.80, 95% CI 1.00-3.22); p=0.047) compared to RA. Use of glucocorticoids, hospitalization, or diabetes did not increase odds of S. aureus carriage. The OA group had decreased odds of S. aureus compared to the RA group; however this was not statistically significant (p=0.987).
Conclusion: RA patients treated with biologics have an increased prevalence of S. aureus colonization. Since nasal S. aureus carriage may play a role in the pathogenesis of surgical infections, S. aureus decolonization should be considered in RA patients on biologics prior to elective surgery.
To cite this abstract in AMA style:
Goodman SM, Shopsin B, Nocon AA, Miller AO, Henry MW, Grond SE, Kaplowitz E, Sculco TP, Russell LA, Donlin LT, Figgie MP, Sculco PK. Staphylococcus Aureus Carriage Rates Are High in Rheumatoid Arthritis Patients on Biologics [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/staphylococcus-aureus-carriage-rates-are-high-in-rheumatoid-arthritis-patients-on-biologics/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/staphylococcus-aureus-carriage-rates-are-high-in-rheumatoid-arthritis-patients-on-biologics/