Session Information
Date: Tuesday, October 23, 2018
Title: Patient Outcomes, Preferences, and Attitudes Poster II: Patient Perspectives
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Shared decision making is key to optimizing management of patients (pts) with psoriatic arthritis (PsA).1 Few studies have evaluated pt preferences for treatment administration across different countries. Qualitative research allows understanding of pt perspectives to help guide this process. This study aimed to understand PsA pt preferences, with pt justification, for treatment administration modes.
Methods: Pt-reported demographic and disease information was obtained at screening with qualitative interviews conducted using a semi-structured interview guide in adult PsA pts with current DMARD (biologic/non-biologic) experience in the US, UK, France, Germany, Italy, Spain, and Brazil. Choice ranking and 100-point allocation tasks were used to evaluate order and strength of preference (0 to 100 [low to high]) across 4 treatment modes: oral (once daily), self-injection (SI; weekly), clinic injection (CI; weekly), and infusion (monthly). Transcripts were in English. Analyses were descriptive (ATLAS.ti v7.5).
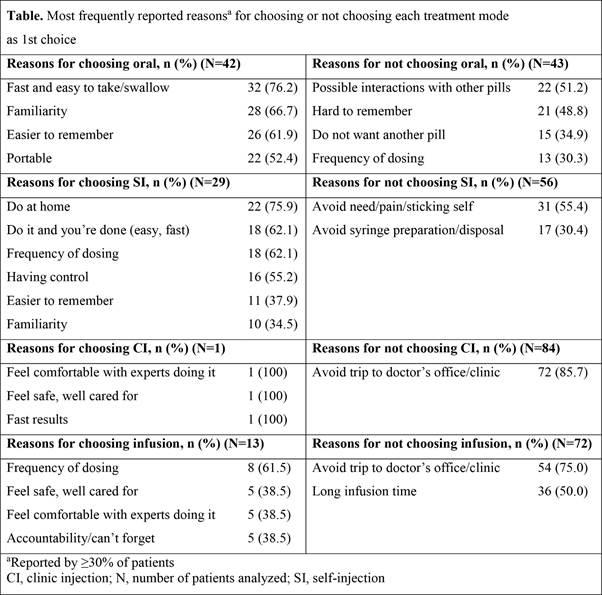
Results: 85 interviews (25 US; 10 in each other country) were conducted (60% female; mean age, 49.6 years; mean age at PsA diagnosis, 39.7 years). Most pts (70.6%) reported moderate/severe PsA with mean joint pain (4.7), fatigue (5.2), and joint/skin severity (5.9) on a 0 to 10 (low to high) numeric rating scale. Most commonly reported symptoms were pain (87.1%), skin plaques (69.4%), stiffness (52.9%), and joint swelling (48.2%). Current PsA treatment mode was oral (62.3%), injection (63.5%), and infusion (5.9%); 80.0% and 29.4% of pts had experience with injections and infusions, respectively. Oral was allocated the highest mean (standard deviation) preference points (43.9 [31.9]) and was more frequently ranked 1st choice (49.4%) vs SI (32.4 [24.8]; 34.1%), infusion (14.5 [20.0]; 15.3%), and CI (9.2 [10.0]; 1.2%). More US than European pts (88.0% vs 38.0%; p<0.001) ranked oral as 1st choice. Overall, 48 (56.5%) pts had a ‘strong’ 1st choice preference (point allocation ≥60); most chose oral (66.7%) vs SI (27.1%), infusion (6.3%), and CI (0.0%). Speed of administration was the most common reason for choosing oral (76.2%; Table) and for SI was home administration (75.9%). The most common reason for not choosing oral was possible interaction with other pills (51.2%) and for SI was to avoid needle pain (55.4%).
Conclusion: More pts preferred oral as a PsA treatment mode followed by SI, and preference for oral was greater in the US than Europe. Reasons for pt preferences included speed/ease of use, safety concerns, feeling of control, and to avoid pain/needles; 56.5% of pts felt strongly about their 1st choice preference. Discussions with health care professionals and/or pt support groups about PsA treatment mode options may help the shared decision-making process for choosing appropriate treatment.
1. Garrido-Cumbrera et al. Rheumatol Ther 2017; 4: 219-31
To cite this abstract in AMA style:
Aletaha D, Husni ME, Merola JF, Ranza R, Bertheussen H, Lippe R, Young P, Cappelleri JC, Brown TM, Ervin C, Hsu MA, Fallon L. Facilitating Shared Decision Making in Psoriatic Arthritis: Factors Influencing Patient Preference for Treatment Mode of Administration [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/facilitating-shared-decision-making-in-psoriatic-arthritis-factors-influencing-patient-preference-for-treatment-mode-of-administration/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/facilitating-shared-decision-making-in-psoriatic-arthritis-factors-influencing-patient-preference-for-treatment-mode-of-administration/