Session Information
Date: Monday, October 22, 2018
Title: 4M087 ACR Abstract: Reproductive Issues in Rheumatic Disorders (1852–1857)
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose:
Pregnancies in systemic lupus erythematosus (SLE) are considered high risk and associated with medical and obstetric complications [1]. Our objective was to study the national trends of obstetric and medical complications in pregnant SLE patients over the past 2 decades.
Methods:
Our study analyzed yearly retrospective trends of cross-sectional data using National Inpatient Sample (NIS) database from 1998 to 2014. Diagnoses and procedures were identified using ICD-9 codes. We included pregnancy-related admissions (diagnosis codes 632-649, 650-669, 670-679, V27, procedure code 72-75) with and without SLE (ICD 9 code 710.0). We studied multiple medical and obstetric complications including maternal mortality, cesarean section, intrauterine fetal death, preeclampsia/eclampsia, length of stay and inflation adjusted hospital charges. Univariable logistic regression was performed to assess temporal trend in SLE and non-SLE pregnancies. Logistic regression with interaction term between SLE and year was performed to detect whether SLE was an effect modifier for our outcomes. Weights were applied to represent the nationwide estimates.
Results:
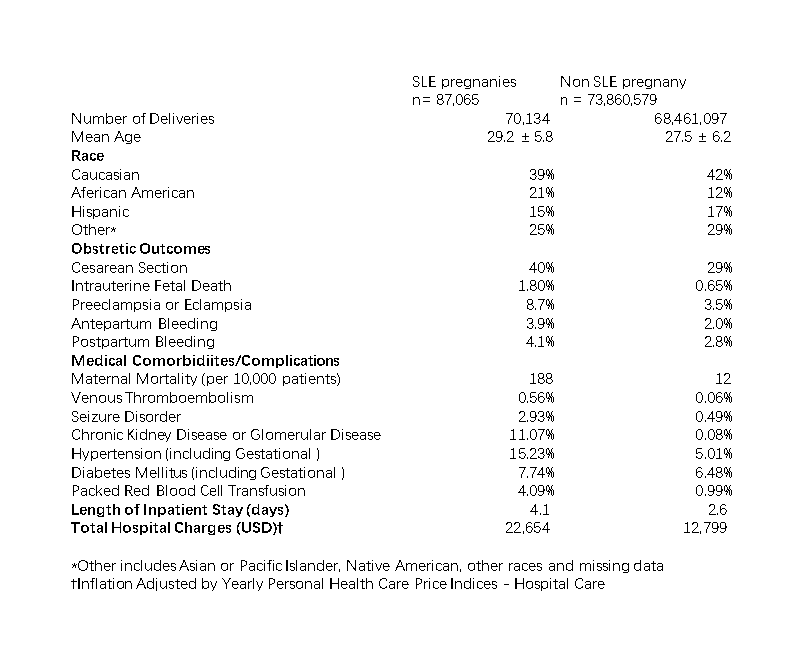
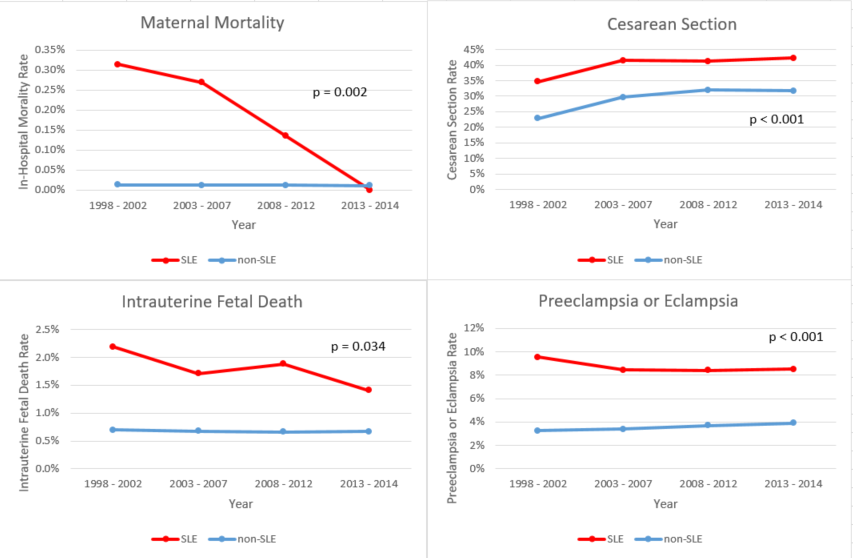
87,065 pregnant women with SLE and 70,162,163 without SLE had hospitalizations in US from 1998 to 2014. Pregnant SLE patients were older (29.2 ¡À 5.8 vs 27.5 ¡À 6.2), had a higher proportion of African Americans (21% vs 12%) and had a higher maternal mortality, and intrauterine fetal death, compared to those without SLE. (Table 1) Increased obstetric as well as maternal complications and comorbidities are observed in SLE patients compared to non-SLE patients. There was a decline in maternal mortality and intrauterine fetal death overtime and this decline was greater in SLE patients compared to those without SLE (p = 0.002 and 0.034, respectively). (Figure 1) There was an increase in cesarean section in both SLE and non-SLE pregnancies and the increase in SLE pregnancies was less than non-SLE pregnancies (p < 0.001). Length of stay decreased in SLE pregnancies however increased in non-SLE pregnancies (p < 0.001). (Table 2)
Conclusion:
Maternal and fetal mortality and important clinical outcomes in SLE pregnancies have improved over the past two decades. This is the largest study of SLE pregnancies in the U.S..
[1] Peart E et al, Curr Opin Rheumatol. 2014
To cite this abstract in AMA style:
Luo Y, Xu J, Mehta BY. Pregnancy in Lupus: 17-Year U.S. Nationwide Trend in Obstetric and Maternal Outcomes [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/pregnancy-in-lupus-17-year-u-s-nationwide-trend-in-obstetric-and-maternal-outcomes/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/pregnancy-in-lupus-17-year-u-s-nationwide-trend-in-obstetric-and-maternal-outcomes/