Session Information
Date: Monday, October 22, 2018
Title: Vasculitis Poster II: Behҫet’s Disease and IgG4-Related Disease
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose:
Pulmonary artery involvement (PAI) is the most common form of arterial involvement in Behçet’s syndrome (BS). A previous survey (1) by our group had analyzed the clinical characteristics and outcome in 47 pts with PAI registered between 2000-2007 and, as compared to our previous experience showed that: 1.the overwhelming male predominance was decreasing; 2. 1/4th of the pts had isolated pulmonary artery thrombosis (IPAT); and 3. the mortality rate was 26% after a mean follow-up of 7 yrs. Recently we had the impression the percentage of female pts was perhaps further increasing; the number of pts with IPAT were increasing and we started to use more biologics. We aim to look at these assumptions formally in a recent group of BS pts with PAI.
Methods:
We reviewed the records of 3390 pts with BS in our multidisciplinary clinic between Jan 2008 and Jan 2018. We identified 47 (42M/5F) pts with PAI and recorded all information regarding clinical characteristics, outcome, radiological studies and treatment.
Results:
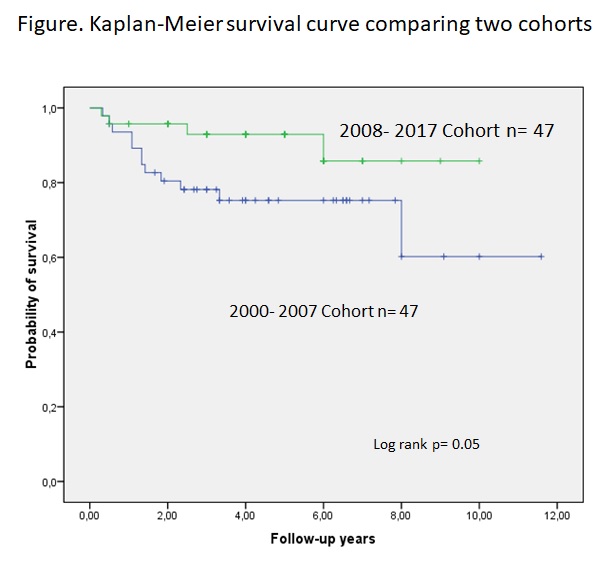
The prevalence of pts with PAI decreased from 1.9% to 1.4% in the recent cohort. The M/F ratio, the mean age at the onset of PAI and the frequencies of other vascular involvement were similar across the 2 cohorts. However, there were more pts with neurological disease in the recent cohort. As usual, PAI were mostly bilateral and involved descending lobar arteries. On the other hand, types of PAI involvement at presentation had changed substantially: those with IPAT reached a share of 45%. Forty-five (96%) pts received cyclophosphamide (Cy) for a mean of 6±4 courses, which was significantly shorter compared to the previous cohort. Twenty-three (49%) pts received anti-TNF because of relapsing course, side effects or unresponsiveness for a mean follow-up of 8±4 mo while only 2 pts received anti-TNF’s in the older cohort. 4 pts had lung surgery, lobectomies in 3 due to giant rapidly progressing aneurysms and a cavitectomy in 1. Bronchial artery embolization was done in 3 pts due to refractory hemoptysis. The outcome of information was available on 45/47 pts: 4 pts (8%) had died, 2 were lost to follow-up after 12 and 16 mo of follow-up and the remaining were alive after a median follow-up of 5 [IQR:3-9] yrs. The causes of deaths were massive hemoptysis in 3, severe pulmonary hypertension in 1. The survival has improved significantly in the recent yrs (figure).
Conclusion:
The surveys of 2 cohorts showed the prevalence of PAI perhaps mildly decreased, IPAT type of involvement was with considerably higher frequency and the outcome was getting better. Cy was still the first agent however its duration of use became much shorter and anti-TNF’s were used in about half of the cohort. The survival seems to have improved significantly. This could have been due to a decreased severity of the type of PAI, with IPAT becoming the most frequent type and or a better management.
1)Seyahi E, Medicine (Baltimore). 2012
To cite this abstract in AMA style:
Ozguler Y, Dincses E, Bakan S, Hatemi G, Melikoglu M, Yurdakul S, Yazici H, Seyahi E. An Update on Pulmonary Artery Involvement in Behcet’s Syndrome: More Pulmonary Artery Thrombotic Disease and a Better Outcome [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/an-update-on-pulmonary-artery-involvement-in-behcets-syndrome-more-pulmonary-artery-thrombotic-disease-and-a-better-outcome/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/an-update-on-pulmonary-artery-involvement-in-behcets-syndrome-more-pulmonary-artery-thrombotic-disease-and-a-better-outcome/