Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose:
C3, the central protein of the complement cascade, participates in an amplification loop that can lead to complement deposition and host tissue damage. If elevated, downstream C3 activation products, including C3a and iC3b, can reflect an underlying tissue inflammation and potential disease activity, such as previously demonstrated in lupus nephritis. Complement 5a, which is preceded by iC3b in the complement cascade, and its receptor C5aR (CD88), are involved in the pathogenesis of anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV). This study examined plasma iC3b levels as a biomarker of active disease in AAV.
Methods:
Data and plasma samples from patients with AAV enrolled in a prospective multicenter longitudinal cohort were utilized for this analysis. The index visit was defined as a time of severe active disease with any new/worse major item, or ³3 minor items, on the BVAS/WG. Plasma iC3b levels were measured at 1-2 visits prior to, and at 1-2 visits after the index visit; all pre and post index visits were at time of remission (BVAS/WG=0). To evaluate the association of the plasma iC3b levels with disease activity, a mixed effect model was used with the biomarker measurement as the outcome, adjusting for ANCA type (c-ANCA/MPO or p-ANCA/PR3), sex, age, race, time to index, and visit type (pre- or post-index). Plasma iC3b levels were log transformed for all analyses.
Results:
Data from 110 patients with active AAV were included. 89% of the patients were Caucasian, and 66% were female. 80% of the patients had GPA with c-ANCA/PR3 positivity, with a median disease duration of 4.1 years at baseline (range 0.2 – 23.8 years). The median Ln (iC3b) at the time of active disease was 1.3 μg/ml (range 0.0 – 4.5 μg/ml). Plasma for measurement of iC3b levels were available for 147 pre-index visits and 161 post-index visits.
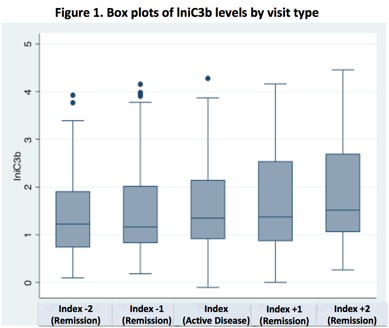
In an adjusted mixed effects model where plasma iC3b level served as the dependent variable, the mean plasma iC3b level at index visit (active disease) was not higher than the mean plasma iC3b level at pre-index visit (p=0.17) or at post-index visit (p=0.37) (Table 1 and Figure 1). In the same adjusted mixed effects model, patients positive for p-ANCA/MPO, had higher levels of plasma iC3b compared to patients positive for c-ANCA/PR3 (p<0.01). Plasma iC3b levels increased for each one year increase in age (p=0.05) (Table 2).
Conclusion:
In AAV, plasma iC3b levels are not associated with disease activity. Older patients and patients with positive p-ANCA/MPO have higher levels of plasma iC3b, possibly indicating increased systemic inflammation in these patients.
Total number of characters: 2241
|
Table 1. Mixed effects models examining the association of lniC3b levels with disease activity (outcome: ln iC3b level) |
|||
|
|
Estimate |
95% CI |
p-value |
|
Visit Type (Ref: Index) Pre-index Post-index |
-0.14 0.09
|
(-0.34; 0.06) (-0.11; 0.29) |
0.17 0.37
|
|
Time to index |
<0.01
|
(-<0.01; <0.01) |
0.13
|
|
Sex (Ref: Female) Male |
-0.12
|
(-0.46; 0.22) |
0.49
|
|
Race (Ref: Caucasian) Non-Caucasian |
0.53
|
(-0.20; 1.26) |
0.16
|
|
ANCA type c-ANCA/PR3 |
-0.56
|
(-0.98; -0.14) |
<0.01
|
|
Age |
0.07
|
(<0.01; 0.13) |
0.05
|
|
CI: confidence interval; Ref: reference group; ANCA: anti-neutrophil cytoplasmic antibody; p: perinuclear; c: cytoplasmic; MPO: myeloperoxidase; PR3: proteinase 3 |
|||
To cite this abstract in AMA style:
E. Najem C, Schmidt M, Stiening C, Cuthbertson D, Carette S, Khalidi NA, Koening CL, Langford C, McAlear CA, Monach PA, Moreland LW, Pagnoux C, Seo P, Specks U, Sreih AG, Ytterberg SR, Merkel PA. Plasma iC3b Level As a Biomarker of Disease Relapse in ANCA-Associated Vasculitis [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/plasma-ic3b-level-as-a-biomarker-of-disease-relapse-in-anca-associated-vasculitis/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/plasma-ic3b-level-as-a-biomarker-of-disease-relapse-in-anca-associated-vasculitis/