Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: ANCA-associated vasculitis including microscopic polyangiitis (MPA) involves multiple organs including lungs. Clinical characteristics and impact on long-term survival in MPA patients with interstitial lung disease (ILD) have not been well characterized. The aim of this study is to clarify clinical characteristics and long-term survival in MPA patients with and without ILD.
Methods: All our patients suspected to have MPA are admitted to our hospital for evaluations. We retrospectively investigated consecutive 76 Japanese patients, classified as MPA with algorithm by Watts, with (n = 44) or without ILD (n = 32) from 2006 through 2014. We compared between-group differences. All patients underwent chest CT.
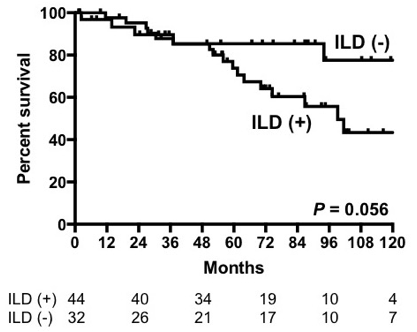
Results: The 76 patients (female, 88%) had mean follow-up period (SD) of 66 (42) months. Mean age (SD) was 71 (8) and 67 (15) in patients with and without ILD, respectively (NS). The frequency of nephritis was lower in patients with ILD (57%) than in those without ILD (84%) (P = 0.01). Eight (18%) and 4 (13%) patients with and without ILD had mononeuritis multiplex, respectively. Treatment in patients with / without ILD included prednisolone alone (with / without ILD, 30% / 41%) or combination with immunosuppressants such as cyclophosphamide (43% / 41%), rituximab (5% / 0%), or azathioprine (23% / 16%). Patients with ILD tended to have low survival compared with those without ILD (P = 0.056). The survival of both groups was similar at the first 4 years. Notably, death in patients with ILD was continuously observed even after 4 years, which was in contrast to those without ILD (figure). Seventeen (39%) and 5 (16%) of patients with and without ILD died during the follow-up, respectively (p = 0.04). Death in 14 patients with ILD (82%) was associated with MPA (n = 8) including deterioration of ILD (n = 5), heart failure (n = 2), and alveolar hemorrhage (n = 1) or with infection (n = 6) including sepsis (n = 3), bacterial pneumonia (n = 2), and pneumocystis pneumonia (n = 1). Among 12 patients with ILD who died after 4 years, death in 9 (75%) patients was associated with lung disease such as deterioration of ILD (n = 6) or infectious pneumonia (n = 3), whereas only one without ILD died from late-stage renal failure. Hazard ratios (HR) for ILD and renal disease were 2.56 (95%CI 0.94-6.97) and 0.89 (95%CI 0.36-2.20), respectively. Patients over age 70 and ILD had independent risk for death (HR 2.61, 95%CI 1.12-6.10).
Conclusion: Death associated with MPA and infections were seen at any period in patients with ILD, which affected the survival. Establishment of more efficient maintenance as well as induction therapy with less side effects is needed in MPA patients with ILD.
To cite this abstract in AMA style:
Matsushita H, Yamasaki Y, Takakuwa Y, Yamada H, Kawahata K. Impact of Interstitial Lung Disease on the Long-Term Survival in 76 Japanese Patients with Microscopic Polyangiitis [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/impact-of-interstitial-lung-disease-on-the-long-term-survival-in-76-japanese-patients-with-microscopic-polyangiitis/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-interstitial-lung-disease-on-the-long-term-survival-in-76-japanese-patients-with-microscopic-polyangiitis/