Session Information
Date: Monday, October 22, 2018
Title: Spondyloarthritis Including Psoriatic Arthritis – Clinical Poster II: Clinical/Epidemiology Studies
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Spondyloarthritis (SpA) is a group of chronic, inflammatory diseases associated with severe pain in the joints and entheses. There is limited evidence on real-world disease burden and treatment patterns in the overall SpA population, as well as individual SpA conditions. This study surveyed self-reported burden of disease and medication use in US patients with SpA in a real-world setting.
Methods: Descriptive data on demographics, disease definition and history, and medication were collected from a random sample of patients with SpA associated with the Spondylitis Association of America (SAA). Between July 7 and August 31, 2017, 820 interviews were conducted with SAA contacts, including 720 completed via Web survey (from 7750 emails) and 100 via follow-up over the phone (from 10,784 phone calls made to 5000 unique numbers). All 820 participants self-reported receiving a diagnosis of SpA from their doctor and were included in this study.
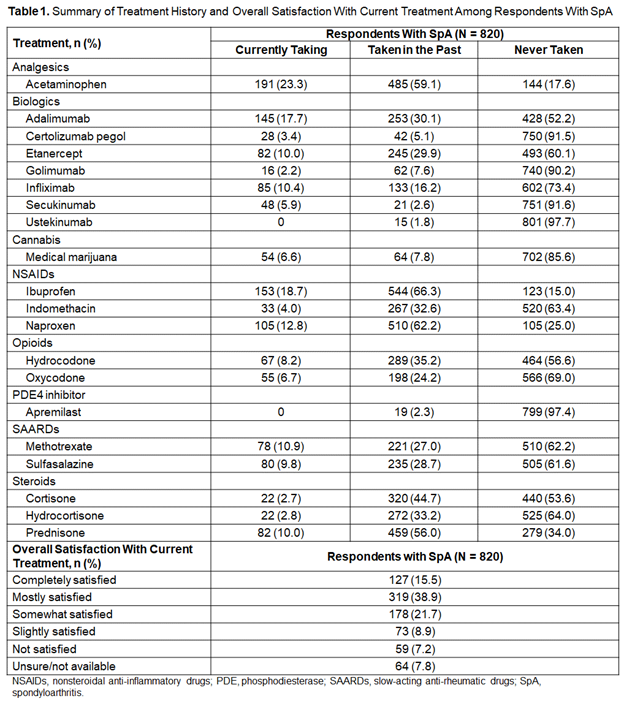
Results: The mean age of the 820 respondents was 55.1 years, and 44.3% were male. The most common self-reported SpA disease was ankylosing spondylitis (AS; 87.3%), followed by uveitis/iritis (28.3%). The most frequently reported comorbidities were high blood pressure (34.8%), high cholesterol (26.5%), and depression (23.4%). Compared with women, men were more impacted by high blood pressure (42.7% vs 28.5%) and heart disease (14.0% vs 4.0%), and less impacted by fibromyalgia (4.2% vs 22.1%). Acid reflux (50.7%) and eye inflammation (45.2%) were also common issues experienced among respondents. On average, respondents with AS first noticed disease symptoms 26.6 years ago, and received an AS diagnosis ≈ 8.2 years later. Respondents saw an average of 2.2 doctors about their back pain, joint pain, or inflammatory problems within the last 2 years, including 20.7% of respondents who saw ≥ 4 doctors. Regarding treatment, 76.7% of respondents with AS received care from rheumatologists, 8.7% from primary care physicians, and 3.8% from orthopedic surgeons; 57.5% of respondents with AS discussed medication options with their doctor and jointly participated in treatment decisions. Prior and current medications are shown in Table 1. More than one-half of respondents (54.4%) were at least mostly satisfied with their current treatment. Many respondents also applied non-medicinal treatment to their lifestyle, including stretching and strengthening exercises (66.2%); biking, running, or walking (57.4%); practicing proper posture techniques (56.5%); and special diets (39.4%).
To cite this abstract in AMA style:
Rosenbaum JT, Pisenti L, Park Y, Howard R. Real-World Insight into the Disease Burden and Treatment of Spondyloarthritis from a US-Based Life Impact Survey [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/real-world-insight-into-the-disease-burden-and-treatment-of-spondyloarthritis-from-a-us-based-life-impact-survey/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/real-world-insight-into-the-disease-burden-and-treatment-of-spondyloarthritis-from-a-us-based-life-impact-survey/