Session Information
Date: Monday, October 22, 2018
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Interstitial pneumonia with autoimmune features (IPAF) has recently been defined to describe patients with interstitial lung disease (ILD) with certain clinical, serologic, and/or morphologic autoimmune characteristics who do not meet criteria for a specific CTD. It remains unclear, however, whether these patients have similar clinical presentations and prognoses to those with CTD-ILD. Our goal was to compare the characteristics of patients with IPAF to those with CTD-ILD, idiopathic pulmonary fibrosis (IPF), and IPF with positive autoantibodies.
Methods: We conducted a retrospective review of patients with ILD enrolled in a single-center, prospective pulmonary cohort from 2012-2017. All patients had undergone a comprehensive clinical, radiographic, and serologic evaluation with an ILD diagnosis established by a multidisciplinary panel including pulmonologists, a radiologist, and a pathologist. We reviewed medical records to collect additional information regarding patients’ rheumatologic history at the time of their initial presentation to our center and identified patients with either: a) IPAF (meeting ≥ 2 of the published clinical, serologic, or morphologic criteria), b) CTD-ILD (meeting established criteria for a CTD) c) IPF without autoantibodies, or d) IPF with autoantibodies (not meeting criteria for IPAF). We compared clinical characteristics, imaging findings, baseline pulmonary function tests (PFTs), and treatment patterns between patients with IPAF and each of the other groups.
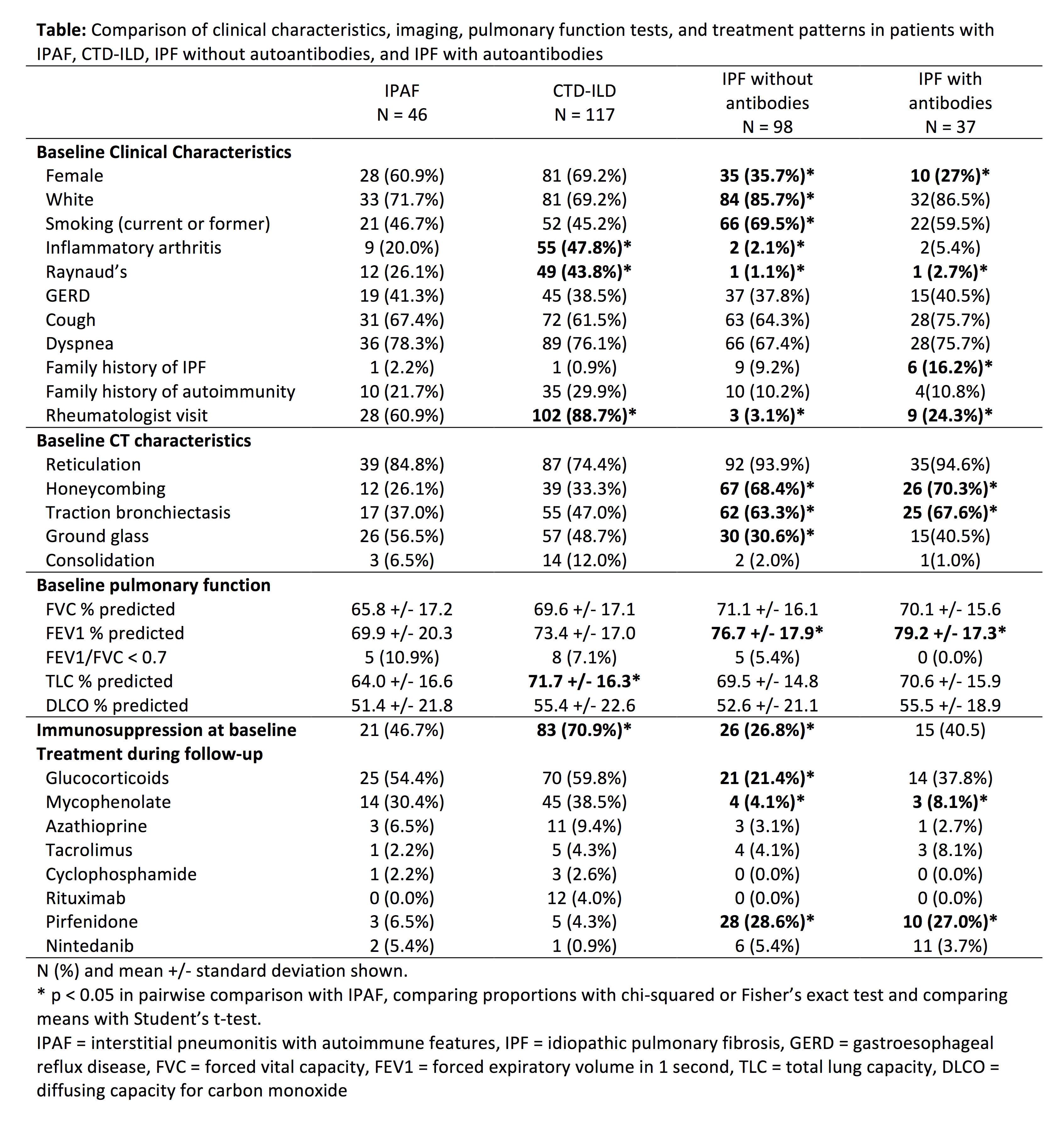
Results: We identified 46 patients with IPAF, 117 with CTD (including 33 RA, 31 SSc, 30 DM/PM, 11 SS), 98 with IPF, and 37 with IPF with autoantibodies. IPAF and CTD-ILD patients were predominantly female and approximately 30% non-white, with similar rates of smoking, family history of autoimmunity, and baseline imaging characteristics (Table). Patients with IPF with or without antibodies were predominantly male and white, more likely to smoke, and less likely to have seen a rheumatologist. Baseline PFTs were similar across the groups. Treatment patterns during follow up were similar in patients with IPAF and CTD-ILD, with >50% receiving glucocorticoids and >30% receiving mycophenolate. A minority of patients with IPF with or without autoantibodies received glucocorticoids during follow-up and >25% of patients in both of these groups received pirfenidone.
Conclusion: Demographic and imaging characteristics were similar among patients with IPAF and CTD-ILD but quite different from those with IPF with or without autoantibodies, supporting the notion of a similar pathophysiology in IPAF and CTD-ILD. IPAF and CTD-ILD patients both commonly received immunosuppression; future work is needed to evaluate whether treatment response is similar in these populations and whether immunosuppression can benefit patients with IPF with positive autoantibodies.
To cite this abstract in AMA style:
Loizidis G, Jiwrajka N, Ligon C, Porteous M, George MD. Clinical Characteristics and Treatment Patterns in Patients with Interstitial Pneumonia with Autoimmune Features (IPAF) [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/clinical-characteristics-and-treatment-patterns-in-patients-with-interstitial-pneumonia-with-autoimmune-features-ipaf/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-characteristics-and-treatment-patterns-in-patients-with-interstitial-pneumonia-with-autoimmune-features-ipaf/