Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Although pain and decreased function are the primary symptom targets of OA surgeries, OA is also associated with depression. The impact of surgery on depressive symptoms is not clear. Further, since 20% or more of patients report residual pain post-surgery, and pain and depression are closely linked, the impact of surgery on depression may vary dependent on pain-related outcomes. The objective our study was to examine patterns of depressive symptoms before and over the year following OA surgery, stratified by 1-year post-surgical outcome and surgical joint. We also examined patterns of patient reported depression diagnoses and treatment.
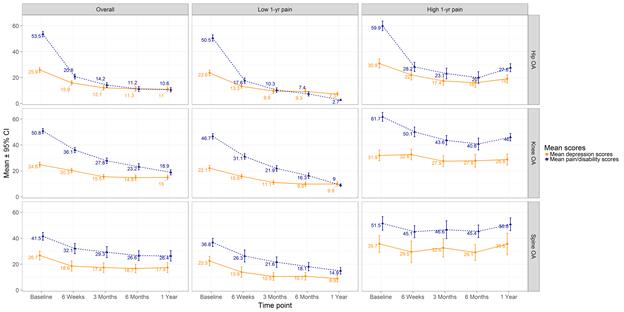
Methods: Participants were 747 patients with hip (n=287), knee (n=360) and lumbar spine (n=100) OA scheduled for joint replacement or decompression surgery +/- fusion. One pre- and 4 post-surgery questionnaires were completed. Depressive symptoms were quantified using the Hospital Anxiety and Depression Scale (HADS). Pain was measured using the WOMAC pain subscale for hip and knee patients. Oswestry Disability Index (ODI) measured disability due to low back pain for spine patients. One-year pain-related outcomes were categorized as ‘high’ (worse) (top pain/disability tertile) vs. ‘low’ (2 lower pain/disability tertiles). Based on the 5 study time points, 2 sets of plots were generated stratified by 1-year outcome and surgical joint:1) mean pain/disability and depressive symptom scores; 2) percentage of patients meeting the HADS cut-off for ‘caseness’ of depression, reporting depression, and reporting current treatment for depression.
Results: Post-surgical changes in mean depression scores varied by joint and 1-year outcome groups. There were notable decreases in depression scores for patients with better pain outcomes across all joint groups. However, for those with poorer outcomes, decreases were smaller for hip and particularly knee patients, and no change was observed among spine patients (Figure). Among those with poorer outcomes, 25% of spine and knee patients were depression ‘cases’ pre- and post-surgery; an additional 16% of spine and 10% of knee patients developed new depression ‘caseness’ post-surgically. The proportion of these knee and spine patients deemed depression ‘cases’ by symptom score was much higher than the proportion reporting depression diagnosis/treatment.
Conclusion: Although depressive symptoms decrease overall in OA patients post-surgery, patterns and degrees of change vary by joint and surgical outcome. Findings support that greater attention to mental health pre- and post-surgery is warranted, particularly among knee and spine patients. Given the close interrelationship of pain and depression, appropriate assessment and treatment of depression in OA patients may lead to decreases in post-surgical pain and improved surgical outcomes, in addition to better overall quality of life.
To cite this abstract in AMA style:
Power JD, Kudesia P, Nadeem A, Perruccio AV, Rampersaud YR, Mahomed N, Gandhi R. Patterns of Depressive Symptoms before and after Surgery for Hip, Knee and Lumbar Spine Osteoarthritis [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/patterns-of-depressive-symptoms-before-and-after-surgery-for-hip-knee-and-lumbar-spine-osteoarthritis/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/patterns-of-depressive-symptoms-before-and-after-surgery-for-hip-knee-and-lumbar-spine-osteoarthritis/