Session Information
Date: Sunday, October 21, 2018
Title: Systemic Lupus Erythematosus – Clinical Poster I: Clinical Manifestations and Comorbidity
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose:
Infection is a leading cause of death and ICU admission in systemic lupus erythematosus (SLE) patients. Our aim was to investigate the outcome and costs of septic shock among SLE patients and to evaluate the main determinants of mortality.
Methods:
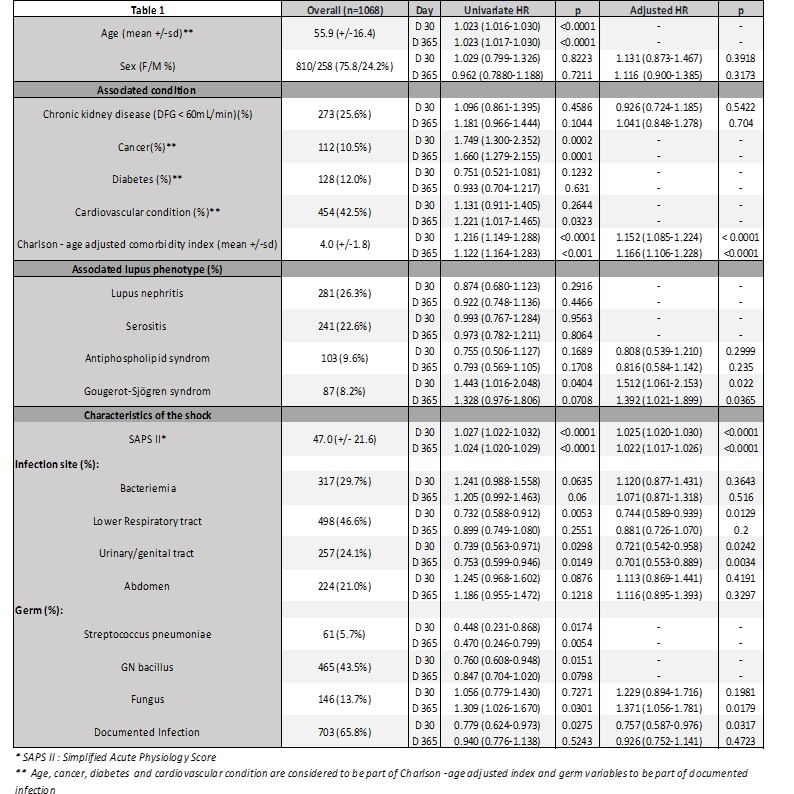
We performed a retrospective analysis of all SLE patients hospitalized with a first episode of septic shock in France from January 1st, 2010 to December 31st, 2015 by extracting data from the PMSI database (Programme de Médicalisation des Systèmes d’Informations) which compiles all data concerning hospital discharges in France. SLE and septic shock diagnoses were based on ICD10 classifications. We assessed the lupus phenotype with diagnostic codes used before or during septic shock hospital stays. Severity of ICU stay was assessed by Simplified acute Physiology score (SAPS II) and procedure use were systematically recorded. Healthcare use and hospital costs were assessed at 1-year for septic shock survivors. Factors associated with 30-day and 1-year in-hospital mortality were studied using Cox regression models. For multivariate analysis, we used sex, chronic kidney disease (CKD) and all variables that had a significance level < 0.20 as covariates.
Results:
One thousand sixty eight (1,068) first ICU stays for septic shock were extracted from 130,150 hospital stays of SLE patients. Inoconstrictors (epinephrine, norepinephrine) were used in 913 (85.6%) patients, invasive mechanical ventilation for 369 (34.6%) and dialysis for 342 (32.0%). Thirty-day and 1-year post admission mortality rates were 30.9 % (n=330) and 43.4% (n=463), respectively. Within one year, 30-day post septic shock survivors (n=738) were re-admitted (mean [SD]) 6.42[17.3] times for 64.1 [48.9] days with a total cost of 14 431€ [20 444€] and 12 (1.6%) required chronic hemodialysis. Factors associated with death are shown in Table1. At 1-year, the main determinants of death were (HR [IC95]) Simplified Acute Physiology Score (SAPS II) (1,022 [1,017-1,026]), Charlson-age adjusted comorbidity index (1,166 [1,106-1,228]), an associated Goujerot-Sjögren syndrome (1,392 [1,021-1,899]) and fungal infection (1,371[1,056-1,781]).
Conclusion:
For SLE patients septic shock is associated with poor short- and long-term outcomes and heavily increased healthcare use at 1-year. We found that independently of severity of the acute illness, Goujerot-Sjögren associated syndrome is a main determinant of 1-year death. Other characteristics of the SLE phenotype were not associated with short and 1-year prognosis.
Table 1: Analysis of first septic shock stays : characteristics and prognosis
To cite this abstract in AMA style:
Mageau A, Sacre K, Perozziello A, Ruckly S, Dupuis C, Bouadma L, Papo T, Timsit JF. Septic Shock Among Patients with Systemic Lupus Erythematosus: Short and Long-Term Outcome and Cost. Analysis of the French Nationwide Database [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/septic-shock-among-patients-with-systemic-lupus-erythematosus-short-and-long-term-outcome-and-cost-analysis-of-the-french-nationwide-database/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/septic-shock-among-patients-with-systemic-lupus-erythematosus-short-and-long-term-outcome-and-cost-analysis-of-the-french-nationwide-database/