Session Information
Date: Sunday, October 21, 2018
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Psoriatic Arthritis (PsA) in a musculoskeletal inflammatory condition associated with psoriasis. It has a heterogeneous set of clinical manifestations which include peripheral arthritis, axial involvement, enthesitis, dactylitis, skin, and nail disease. In current practice, the treatment of PsA involves initiating a conventional synthetic DMARD (csDMARD), usually followed by an initial Tumor Necrosis Factor inhibitor (TNFi) and then a second TNFi before considering other classes of biological DMARD (bDMARD). The efficacy of TNFi in patients with PsA is documented in randomized clinical trials (RCTs) for several of these agents, including etanercept (ETA), infliximab, adalimumab, golimumab, and certolizumab, compared with placebo. However, little is known about the utility of combining a TNFi with MTX (C) versus TNFi monotherapy (M) in psoriatic arthritis and studies to this day show conflicting results. We evaluate here the comparative sustainability of ETA used in first or second intention in patients with PsA initially treated in C or M.
Methods: Data from all RHUMADATA® patients with PsA prescribed ETA either as an initial or second TNFi was analyzed. Patients were followed until treatment discontinuation, loss to follow-up or February 21st, 2018. Only patients who were treated for at least six months were included. The characteristics of selected patients were tabulated, and the ETA discontinuation rates of patients who initiated C and M were compared using Kaplan-Meier estimates and multivariate Cox models adjusting for potential confounders.
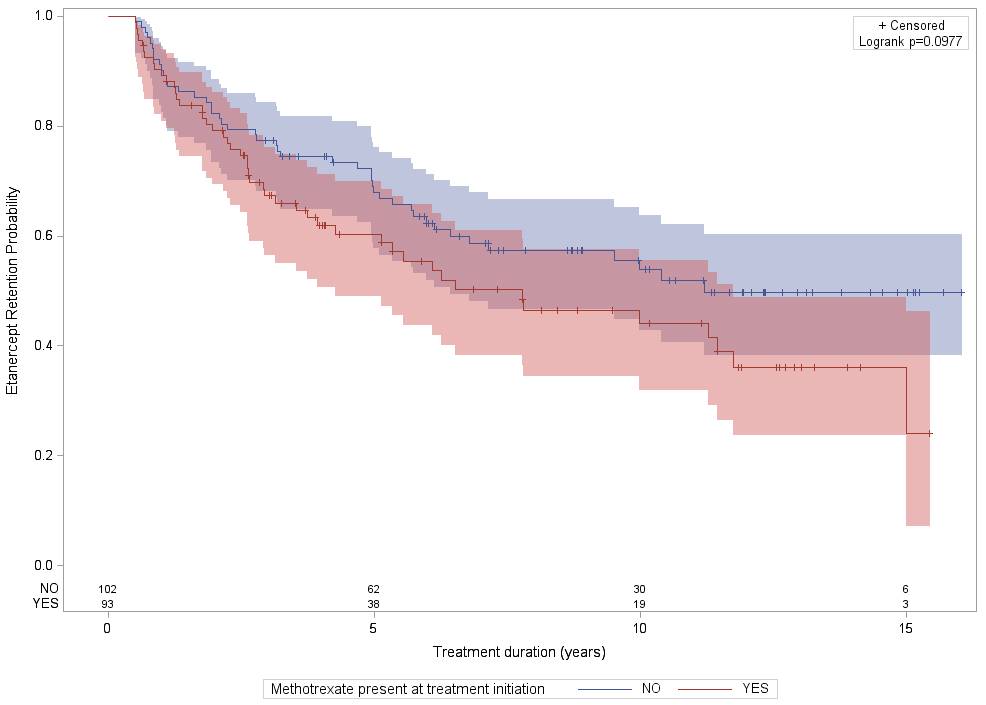
Results: A total of 195 patients with PsA (according to CASPAR criteria) received ETA in first or second intention. Of those, 102(52.3%) and 93(47.7%) received treatment without and with MTX respectively. There were statistically significant differences in populations in table 1 for the BASDAI (M: 5.8±2.8; C: 3.9±2.3; p=0.03) and BASFI (M: 5.0±3.0; C: 2.8±2.0; p=0.011) scores, both being higher in the M group. No significant differences in retention rates between M and C therapy were observed (see figure below). Mean retention time for M and C therapy were respectively 7.12(SE=0.42) and 8.25(SE=0.68) years. The main reason for treatment cessation was inefficacy, followed by adverse events. There were more adverse events in the C group (26.1% vs 9.3%). Sub-analysis looking at ETA in first and in second intention showed similar results.
Conclusion: Combining MTX to ETA does not improve sustainability in patients with PsA.
To cite this abstract in AMA style:
Benryane O, Coupal L, Choquette D. Combining Etanercept with Methotrexate Does Not Improve Long Term Sustainability in Patients with Psoriatic Arthritis. Real World Evidence Report from the Quebec Database Rhumadata® [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/combining-etanercept-with-methotrexate-does-not-improve-long-term-sustainability-in-patients-with-psoriatic-arthritis-real-world-evidence-report-from-the-quebec-database-rhumadata/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/combining-etanercept-with-methotrexate-does-not-improve-long-term-sustainability-in-patients-with-psoriatic-arthritis-real-world-evidence-report-from-the-quebec-database-rhumadata/