Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Early diagnosis for rheumatic conditions is crucial for children to achieve the best functional outcomes. Access to care is difficult due to the volume of referrals and paucity of pediatric rheumatologists. This compelling need to expediently triage dire and complex rheumatology referrals has been painfully demonstrated in our clinic. When this project was initiated there was a 3-month backlog to see a new referral. During this time, several patients were assigned delayed appointment dates due to our lack of a triage process. Improving the referral process so that the appropriate patient is seen quickly is important for early diagnosis and earlier treatment, which improves quality of care for children with chronic debilitating rheumatic conditions.
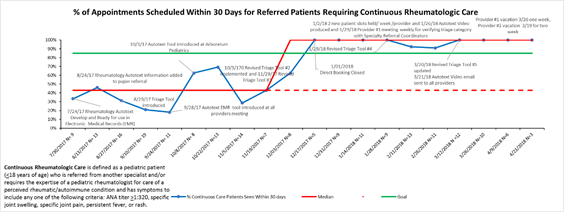
Methods: Our goal was to increase from 35% to 85% our rate of appointments scheduled within 30 business days for referred pediatric patients who require continuous rheumatologic care by June 1, 2018. The quality improvement methodology used for this project was the Model for Improvement with rapid Plan, Do, Study, Act cycles. We defined current state by collecting baseline data, completing a root cause analysis, and surveying staff and patients to identify the most common and impactful failures.
We used a Key Driver Diagram to define our leading factors and guide our change ideas, and an aim statement and data management plan to guide the work and data collection. Our run chart captures biweekly change and demonstrates improvement over time.
Results: The greatest barriers identified during this process each required multiple PDSA cycles to refine and achieve their current state. By addressing the greatest barriers of lack of a standardized referral and triage process, lack of available appointments for higher acuity patients, and limitations in staff and families’ ability to make contact, this team streamlined processes to increase efficiency and throughput while enhancing teammate engagement and improving the health of this at-risk population.
The average number of patients scheduled within 30 days of referral over the first four months compared to the subsequent five months represents a 131% increase. Our run chart shows a shift demonstrating non-random variation and improvement in our outcome measure. We have continuously met and exceeded goal of 85% since December 2017.
Conclusion: Improvement science offers a methodology to strategically address inefficiencies and communication barriers, ensuring improved quality and safety, as well as better patient experience.
By investing time in creative problem-solving, streamlining, and clear communication, and by facilitating staff empowerment and ownership, this project achieved remarkable gains in patient access and care delivery. This result is a process that can be transferred to other settings, and holds great value given the universal challenges of supply/demand.
To cite this abstract in AMA style:
Vora SS, Buitrago-Mogollon TL, Mabus SC, Griffin TA, Sherrod A, Kalhagen LW, Ogletree ES. Snap Crackle Pop: Healing the Cracks in Our Referral Process, Helping Pediatric Rheumatology Patients Get Care Sooner [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/snap-crackle-pop-healing-the-cracks-in-our-referral-process-helping-pediatric-rheumatology-patients-get-care-sooner/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/snap-crackle-pop-healing-the-cracks-in-our-referral-process-helping-pediatric-rheumatology-patients-get-care-sooner/