Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose:
Rheumatoid arthritis (RA) increases the risk of bone density abnormalities such as osteoporosis, predisposing patients to fragility fractures and subsequent morbidity. Osteoporotic fractures incur an economic burden reaching nearly $17 billion annually. Consequently, rheumatologists should assess and manage bone health more attentively. Bone density assessment in RA patients is not always evaluated in routine clinical practice despite guidelines suggesting its importance. We have noted that trainees in the rheumatology clinic are not routinely documenting or managing bone health in our patients. The aim of this quality improvement project was to increase documentation of bone health in RA patients seen by residents and fellows in a high volume VA Medical Center outpatient rheumatology clinic from the baseline 3 month average of 58% to 70% (stretch goal 80%) during the time period of February to April 2018.
Methods:
Pre-intervention documentation rate of bone health was measured by reviewing 50 fellows’ and 50 residents’ rheumatology RA clinic visit notes between August and October 2017 at a VA center serving a large metropolitan area. Patients seen by the authors were excluded. Intervention: In December 2018, a “Bone Health” prompt was added to the RA note template, reminding physicians to document bone health status, FRAX score, and recommendations (Image 1). In order to facilitate the intervention, fellows were educated about the importance of bone health documentation and informed about the QI project at a Grand Rounds conference. Additionally, flyers reminding all residents and fellows about the template were posted in exam rooms at the VA. Post-intervention data were collected between February and April 2018, using the same process.
Results:
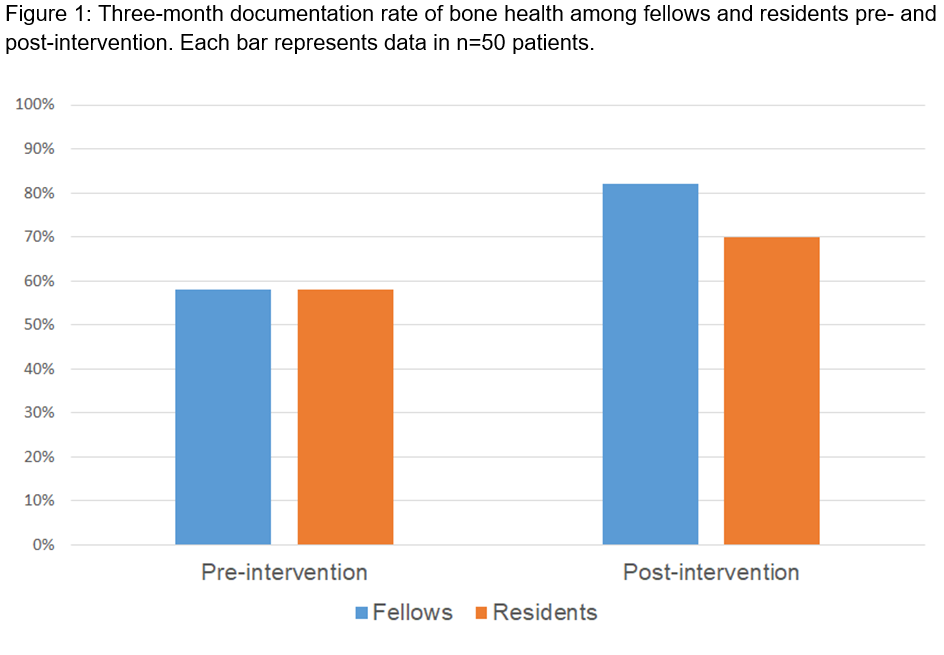
The pre-intervention documentation rate among both 1st and 2nd year rheumatology fellows and residents (Internal Medicine, PM&R) was 58%. The post-intervention rate improved among both fellows and residents to 82% and 70% respectively (n=50 patients per subgroup), meeting the set goal of our project (Fig 1).
Conclusion:
Adding a “Bone Health” prompt to the RA office visit template improves the documentation rate of bone health, as shown by improvement in the post-intervention chart review. Fellows had a greater documentation rate in their post-intervention results than did residents, potentially due to more frequent exposure to this topic. In the future, we plan to analyze if the increased documentation rate translated into improved rates of guideline concordant management of decreased bone density in this vulnerable population.
To cite this abstract in AMA style:
Ahmed B, Nayfe R, Udupa A, Makris UE, Arora R, Reddy S. Documenting Bone Health for Veterans with Rheumatoid Arthritis in an Outpatient Academic Clinic [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/documenting-bone-health-for-veterans-with-rheumatoid-arthritis-in-an-outpatient-academic-clinic/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/documenting-bone-health-for-veterans-with-rheumatoid-arthritis-in-an-outpatient-academic-clinic/