Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: While inflammatory bowel disease (IBD) is a well-known comorbidity in axial spondyloarthritis (SpA), little is known about functional bowel problems, such as irritable bowel syndrome (IBS), in these patients. In the general population, the IBS prevalence has been estimated to be around 11%.[1] In the present study, we examined the frequency of IBS-symptoms and their relation to patient-reported outcomes in an ongoing survey of axial SpA patients.
Methods: Consecutive axial SpA patients were examined and classified as non-radiographic axial SpA (nr-axSpA; ASAS criteria; n=37) or ankylosing spondylitis (AS; modified New York criteria; n=68). Patients with known IBD were excluded. The ROME III questionnaire was used to assess IBS criteria fulfillment,[2] and faecal (F) calprotectin was measured by a commercially available ELISA kit.
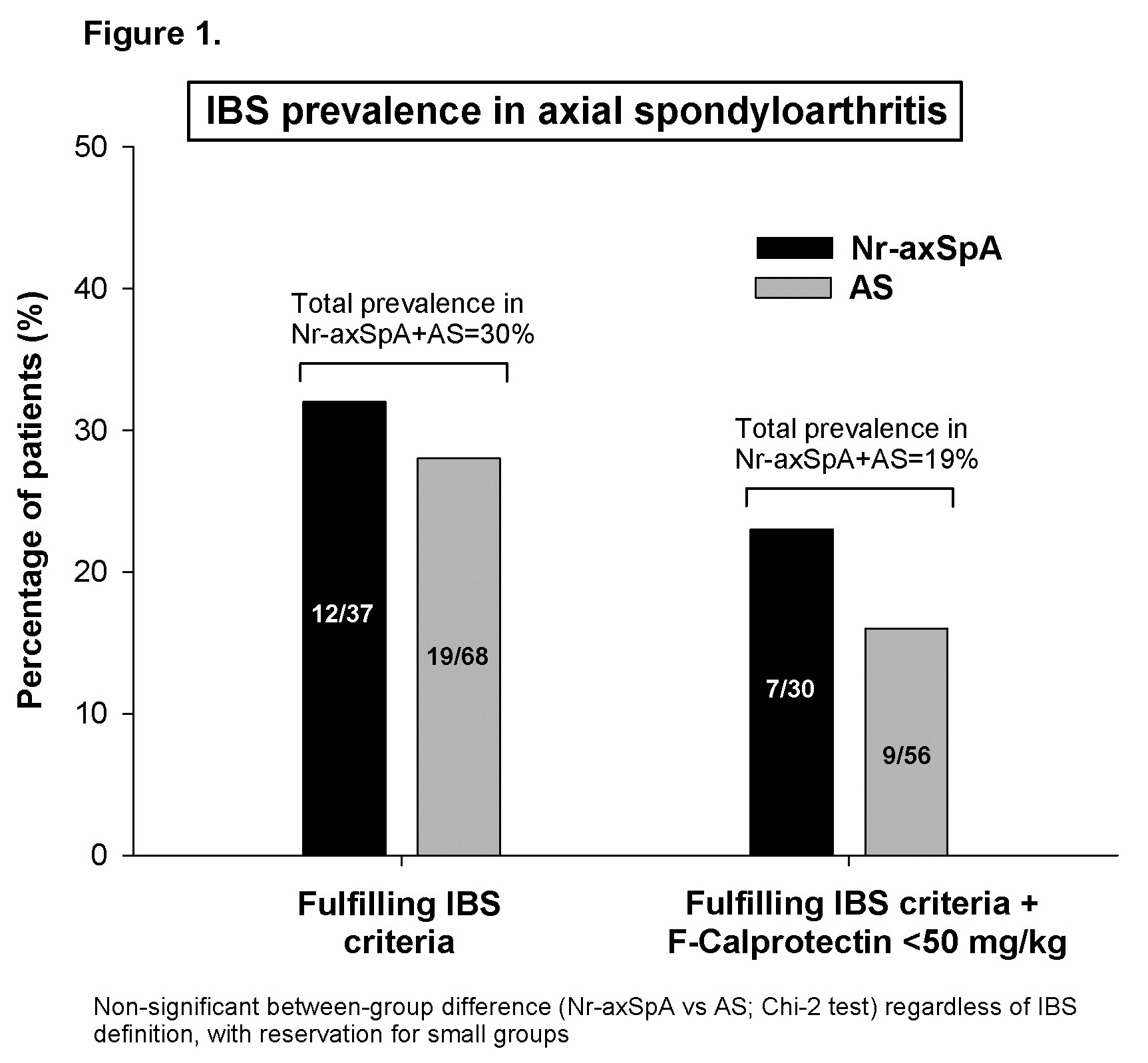
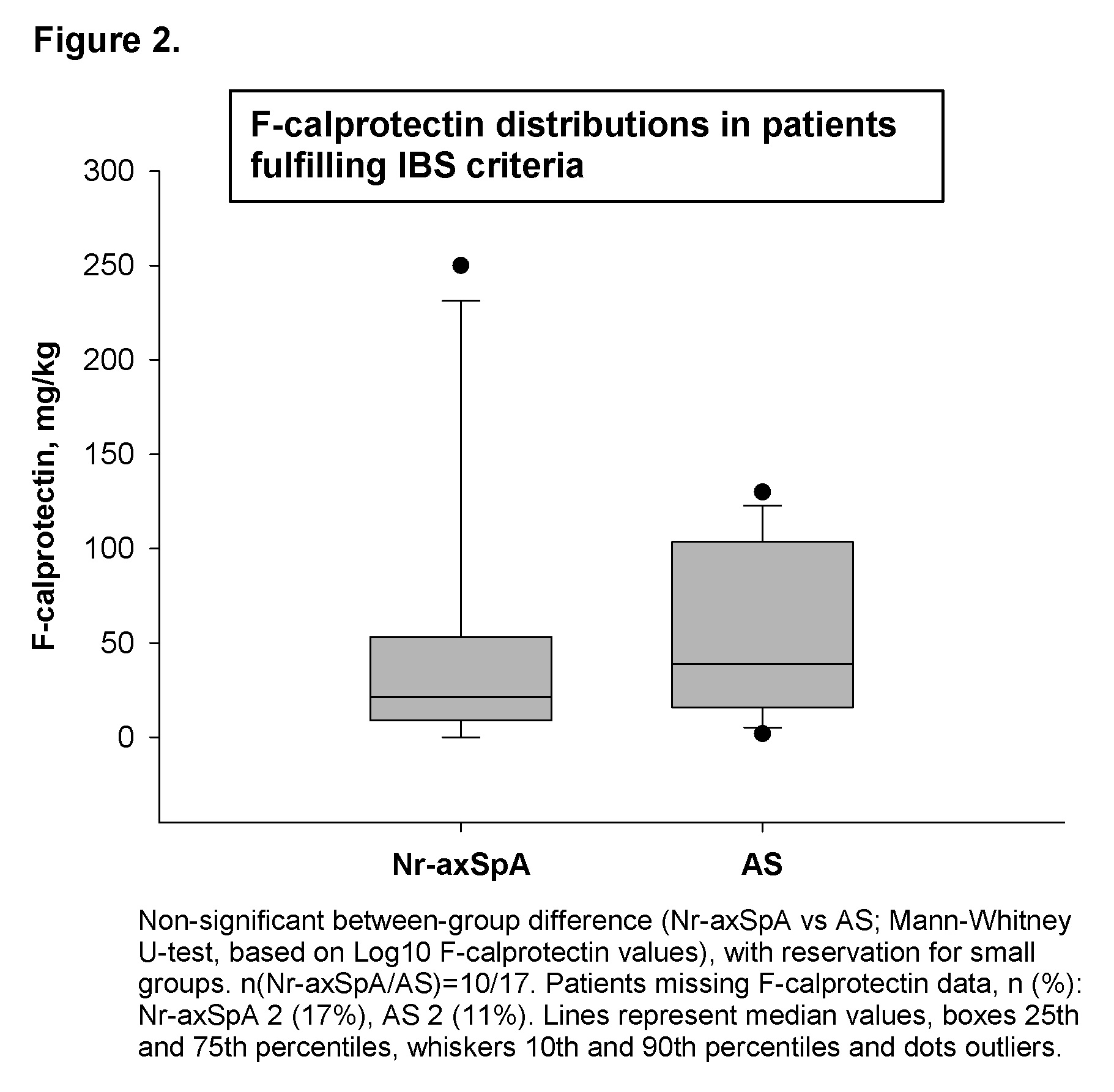
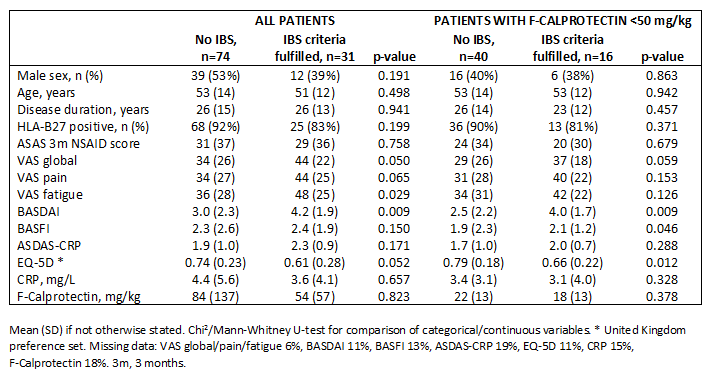
Results: Overall, 30% of patients fulfilled the IBS criteria (n=31; 32%/28% of nr-axSpA/AS patients, no significant between-group difference; Figure 1). In 11 of these subjects (35%), F-calprotectin was, however, also elevated (≥50 mg/kg; F-calprotectin was available in 86 of the 105 patients; Figure 2), making it hard to rule out inflammation rather than functional disease as cause of the symptoms. Applying a stricter definition of IBS, i.e. a combination of fulfilled IBS criteria and a non-pathologic F-calprotectin level (<50 mg/kg), this was met by 19% of the patients (n=16; 23%/16% of nr-axSpA/AS patients, no significant between-group difference; Figure 1). Irrespective of F-calprotectin levels, the presence of IBS symptoms was associated with worse patient-reported outcomes, especially regarding disease activity and health-related quality of life (Table).
Conclusion: In axial SpA patients without known IBD, IBS-symptoms were substantially more common than described for the general population, affecting almost 1/3 of patients, and were linked to worse patient-reported outcomes. To establish the true IBS prevalence in the cohort would require colonoscopy of certain subjects, although even based on a highly conservative definition (fulfillment of IBS criteria and F-calprotectin <50 mg/kg) the observed prevalence was >1.5 times higher than that reported in the general population.
1. Lovell RM, et al. Clin Gastroenterol Hepatol. 2012;10:712-721
2. Drossman DA. Gastroenterology 2006;130:1377-90
To cite this abstract in AMA style:
Olofsson T, Mogard E, Marsal J, Geijer M, Kristensen LE, Lindqvist E, Wallman JK. Irritable Bowel Syndrome and Its Impact on Patient-Reported Outcomes in Axial Spondyloarthritis: Is It an Overlooked Comorbidity? [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/irritable-bowel-syndrome-and-its-impact-on-patient-reported-outcomes-in-axial-spondyloarthritis-is-it-an-overlooked-comorbidity/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/irritable-bowel-syndrome-and-its-impact-on-patient-reported-outcomes-in-axial-spondyloarthritis-is-it-an-overlooked-comorbidity/