Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose:
In a real clinical setting of RA outpatients, we previously showed that musculoskeletal ultrasound (MUS) added to clinical evaluation impacted the treatment decision in 20% of the clinical scenarios evaluated; the impact was greater for the trainee in rheumatology (TR) than for the senior rheumatologist (SR). The aim of the present study was to explore if the results could be generalized to a higher number of physicians.
Methods:
The population of physicians consisted of 10 SR (mean age: 46.2± 12.7 years, 3 of them with ²5 years of experience, 4 with 6-14 years and 3 ³15 years) and 12 TR (median age: 30.8±1.3 years); 94% and 16.7% of the TR and the SR, respectively, referred theoretical MUS training.
10 clinical vignettes included data abstracted from 10 RA outpatients, randomly selected from an ongoing cohort. Each vignette was shared with 6 TR and 6 SR, who were asked to give a first treatment recommendation based on Òtraditional rheumatic assessmentsÓ and in a second step, to confirm or not their previous recommendation after MUS findings were incorporated to the rheumatic assessments.
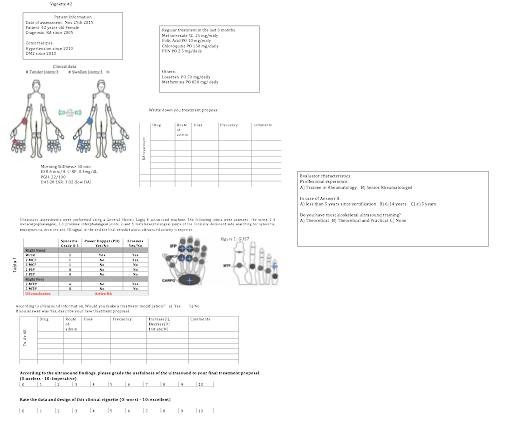
Each vignette included the following data: in the first sheet, patient socio-demographic characteristics, comorbidities, extended disease activity evaluation, previous RA treatment, comorbid conditions treatment and a space for the first treatment recommendation; in the second sheet, MUS information and a space for eventual RA specific treatment changes (Figure).
Results:
Patients were middle-aged females (41.9±7 years old) with (mean±SD) disease duration of 7.5±3.4 years. Six of them had DAS28-ESR remission.
MUS added to the clinical evaluation induced a treatment modification in 26% of the 96 clinical scenarios evaluated, with similar percentage in TR (29.2%) and SR (22.9%), (p=0.64). Within SR, the lesser experienced rheumatologist (<15 years) changed their treatment proposal after MUS finding more frequently (44%) than those with ³15 years of experience (0%, p=0.002); training in MUS did not impact treatment modifications.
MUS induced more treatment modifications in those clinical scenarios with DAS28-ESR active disease vs. remission patients 68% vs 32%, p=0.005. There was a higher (albeit not significant) percentage of disagreement in disease activity level between DAS28 and MUS in active vs. remission patients: 75% vs. 32.8%, p=0.51). Then, we identified 48 clinical scenarios (50%) with disagreement in disease activity as per DAS28 and per MUS; of them 18 (37.5%) were in DAS28-ESR remission and 30 had active disease; there were a higher percentage of treatment modifications after MUS information was incorporated to clinical data in active clinical scenarios vs. remission clinical scenarios: 43.3% vs. 11.1%, p=0.026.
Conclusion:
The impact of adding MUS to clinical evaluations in the treatment decision of RA patients is affected by physician experience and disease activity status.
To cite this abstract in AMA style:
Sifuentes-Cantú C, Contreras-Yañez I, Gutierrez M, Pascual-Ramos V. Physician Experience and Patient´s Disease Activity Affect the Impact of Musculoskeletal Ultrasound on the Treatment Decision in Rheumatoid Arthritis Patients [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/physician-experience-and-patients-disease-activity-affect-the-impact-of-musculoskeletal-ultrasound-on-the-treatment-decision-in-rheumatoid-arthritis-patients/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/physician-experience-and-patients-disease-activity-affect-the-impact-of-musculoskeletal-ultrasound-on-the-treatment-decision-in-rheumatoid-arthritis-patients/