Session Information
Date: Monday, November 6, 2017
Title: Systemic Sclerosis, Fibrosing Syndromes and Raynaud's – Clinical Aspects and Therapeutics Poster II
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Renal Resistive Index (RRI), measured by Doppler ultrasound, reflects changes in both renal vascular and tubular-interstitial compartments and systemic vascular compliance related to age and comorbidities (arterial hypertension, diabetes, hyperuricaemia, etc). As renal injury in younger decades may occur also for RRI <0.70, the use of this cut-off may underestimate. RRI was previously investigated in small SSc samples not considering possible confounding medical conditions. The objectives of the study were: to describe RRI in our SSc population, to test both fixed 0.70 RRI cut-off and SSc-age-adjusted cut-offs in reflecting renal and other organ involvement, to analyse the prognostic value of baseline RRI and RRI Δ change in predicting clinical worsening.
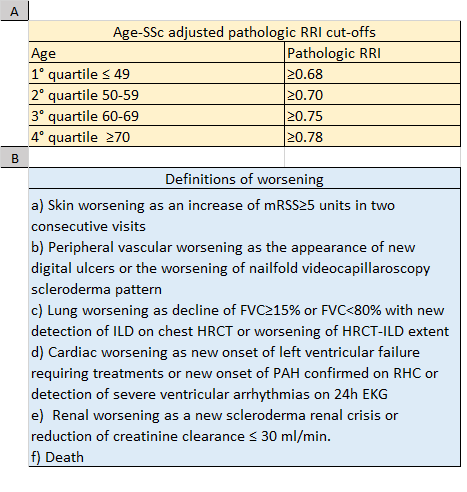
Methods: SSc patients classified through ACR/EULAR 2013 criteria, ≥18 years were enrolled after informed consent. Baseline Data on RRI, laboratory, instrumental and therapeutic features were retrospectively collected. SSc-age-adjusted pathologic cut-offs were created dividing the population in age quartiles and considering RRI values >75th percentile as pathologic (Table 1A). Clinical worsening was defined in case of any event listed in Table 1B. Data were analysed as appropriate with SPSS vers. 20.0.
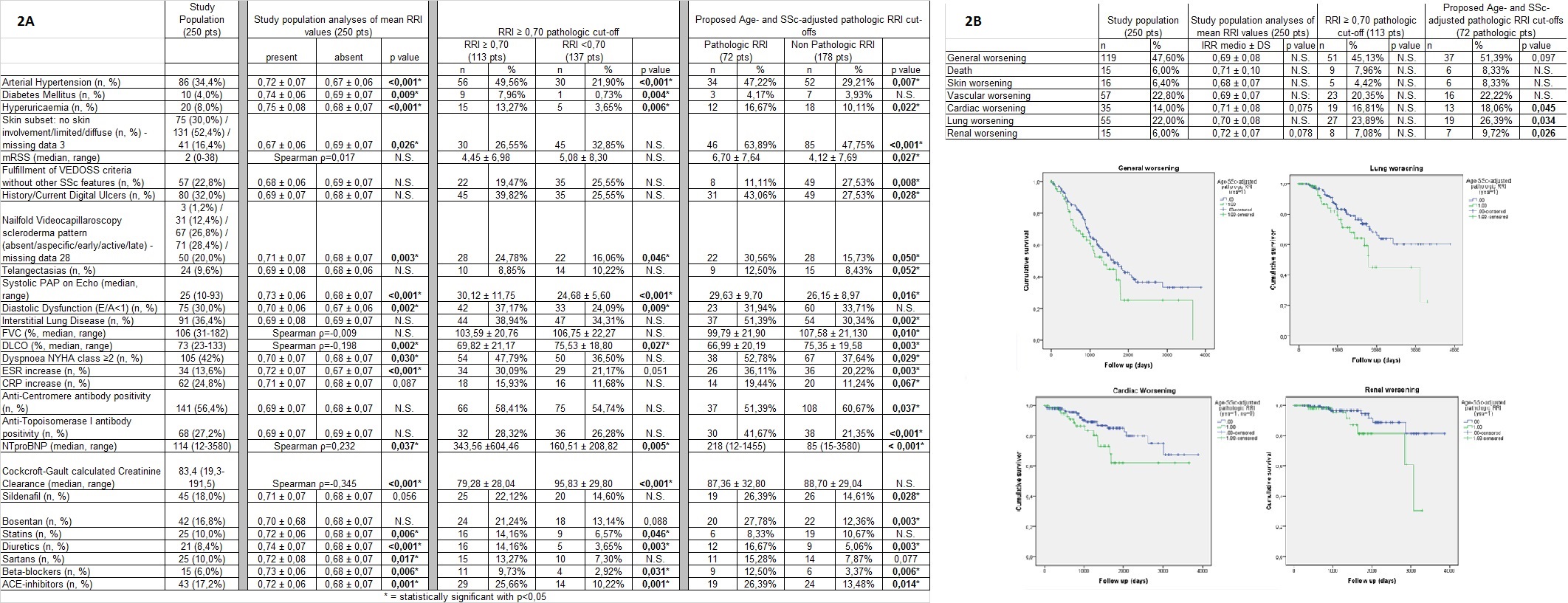
Results: 250 SSc patients (mean disease duration 7.2±8.3 years) were eligible. RRI showed significant correlations with age (ρ=0.56, p<0.001) and creatinine clearance (ρ=-0.38, p<0.001), as well as significant associations with general population RRI determinants. When considering RRI absolute value and 0.70 cut-off, only comorbidities, renal function, sPAP and E/A, DLCO and late NVC pattern were associated. Conversely, new SSc-age-adjusted RRI cut-offs could not detect early renal damage but were significantly associated with various disease related skin and lung fibrotic manifestations, as well as vasculopathic complications (Table 2A). After a mean follow-up of 3.6±2.6 years, while RRI absolute values and 0.70 RRI cut-off showed no significant value, SSc-age-adjusted RRI cut-offs were significantly predictive for cardiac, lung and renal worsening (Table 2B). On the other hand, RRI Δ changes in 3 years (100 pts) and 5 years (60 pts), were not sensitive or predictive for worsening.
Conclusion: in clinical practice, different age-SSc-adjusted or non-adjusted RRI cut-offs may be used to evaluate renal and extrarenal involvement, resembling DLCO for parenchymal and vascular lung involvement. These RRI cut-offs may be considered as possible predictors of kidney, lung and cardiac worsening in SSc patients.
To cite this abstract in AMA style:
Bruni C, Maestripieri V, Tesei G, Chiostri M, Guiducci S, Bellando-Randone S, Boddi M, Matucci-Cerinic M. Different Cut-Offs for Renal Resistive Index Reflect Renal and Other Organ Involvement and Predict Worsening in SSc Patients [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/different-cut-offs-for-renal-resistive-index-reflect-renal-and-other-organ-involvement-and-predict-worsening-in-ssc-patients/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/different-cut-offs-for-renal-resistive-index-reflect-renal-and-other-organ-involvement-and-predict-worsening-in-ssc-patients/